By Dr. Lev Kalika, owner of New York Dynamic Neuromuscular Rehabilitation & Physical Therapy in New York City, special to SportsMD.com

Gender equity in athletics has long been a raging battle, with male athletes dominating in media attention, scholarships and pay. In 1972, Title IX of the Educational Amendments of 1972 was added to the Civil Rights Act of 1954, stating that, “No person in the United States shall, on the basis of sex, be excluded from participation in, be denied the benefits of, or be subject to discrimination under any educational program or activity receiving federal financial assistance.”
While Title IX opened many doors for female athletes in both sports and academics, there remain significant disparities in the treatment and compensation of female athletes. A notable recent example is the controversy in professional league soccer over women’s matches being played mostly on artificial turf, while men’s teams play on natural turf. Artificial turf is known to increase injury risk, especially injuries of the sort that are more commonly suffered by female players, like ACL ruptures.
During the recent FIFA Women’s World Cup, it was hard to ignore the cries from fans for equal pay for female athletes. Injuries can be career-ending, and equitable pay helps to offset medical expenses and other long-term repercussions of injury.
Gender Bias in Athletic Injury Treatment

The disparity in treatment between male and female athletes is also evident in injury management. There are distinct and significant anatomical and biological differences between men and women, yet female athletes are often assessed, diagnosed and treated by standards identical to those applied to their male counterparts. In fact, the anatomical model used in sports medicine is male. Yet female athletes are more prone to certain types of sports injuries than males playing the same sports.
Among the most common injuries in female athletes are;
- rotator cuff (shoulder) injuries
- knee injuries
- ankle injuries
- stress fractures
- plantar fasciitis

In sports medicine, gender bias exists across the board, from a dearth of female participants in research studies, to decision-making about female health, training and performance based on data from male-dominated clinical trials. Even pharmaceutical drugs are most often developed and tested using primarily male subjects, despite significant hormonal and biological differences between men and women.
It is important to note that female athletes are not the only patients harmed by gender bias. Male athletes may also be misdiagnosed, under-treated or released to return to play prematurely due to gender-biased assumptions. This bias has its roots in social, cultural and even political influences, and can only be eradicated by changes in the way we approach, train, diagnose and treat both female and male athletes.
Sports Injury Incidence and Outcomes
 In both male and female athletes, the most common sports injuries include bone stress fractures, injuries to the anterior cruciate ligament (ACL) and concussions. While research comparing male vs female injury incidence and outcomes is limited, there is a growing body of evidence suggesting that female athletes are at higher risk of injury, and are likely to report injuries at a significantly higher rate than males participating in the same sports.
In both male and female athletes, the most common sports injuries include bone stress fractures, injuries to the anterior cruciate ligament (ACL) and concussions. While research comparing male vs female injury incidence and outcomes is limited, there is a growing body of evidence suggesting that female athletes are at higher risk of injury, and are likely to report injuries at a significantly higher rate than males participating in the same sports.
- Concussion: In a review of 10 years of data published in the British Journal of Sports Medicine, female athletes appear to be at greater risk for concussion than male athletes in the same sports, and experience more severe symptoms of traumatic brain injury and concussions. Another study published in the Journal of Athletic Training found that female athletes sustained a higher percentage of concussions during games than male athletes, with the highest concussion rates occurring in women’s soccer.
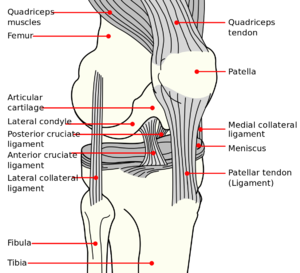
- ACL Injuries: In a a 5-year evaluation of anterior cruciate ligament injuries in collegiate men’s and women’s soccer and basketball programs, female athletes incurred significantly higher rates of ACL injuries in both sports compared to males.
- Bone Stress Injuries: Stress fractures in female athletes have long been associated with the female athlete triad, marked by inadequate energy intake and menstrual dysfunction leading to reduced bone mineral density and increased risk of bone fractures. Recently, research has revealed that low energy availability (EA) coupled with intense training levels also affects male athletes, lowering testosterone levels and increasing the risk of bone fractures.
Characteristics Contributing to Injury in Female Athletes

There are multiple biological differences between male and female athletes that may account for differences in injury incidence.
Specific differences in female athletes include:
- higher estrogen levels,
- higher fat to lean ratio
- lower center of gravity
- greater joint flexibility due to looser ligaments and lower muscle strength
- wider pelvis that alters hip-knee-ankle alignment
- smaller knee joint capsule, with narrower space for the ACL
- hormonal fluctuations throughout the menstrual cycle that affect injury risk
- altered muscle activation patterns during landing and directional changes

Differences and similarities in injury incidence in male and female athletes indicate a need to reevaluate how we train, assess, diagnose and treat athletes. If we are to continue to improve performance while lowering injury risk, gender bias and stereotypes must be laid aside, and each athlete must be treated as an individual, taking into account sex, nutritional status, training approaches and other factors that impact injury risk.
Implications for Rehabilitation
In the rehab sphere, there is a growing need for therapists with an in-depth understanding of female anatomy and how it is impacted by force loads during sports. Anatomical distinctions between men and women should be taken into consideration when devising treatment protocols and training regimens for return to sport.
Athletes should be assessed, diagnosed, treated and retrained on a case-by-case basis, taking into consideration the unique needs of each athlete. Already, timetables for return to play are giving way to more specific measures of readiness, both physically and mentally.
Individualized and unbiased diagnosis and treatment can help injured athletes return to play with confidence. Taking gender differences into account when designing training programs can mitigate the risk of injury and help each athlete realize his or her performance potential.
Resources
Covassin, Tracey et al. Sex differences and the incidence of concussions among collegiate athletes. Journal of Athletic Training 2003; 38(3): 238-244.
Dick, RW. Is there a gender difference in concussion incidence and outcomes? British Journal of Sports Medicine 2009;43:i46-i50.
