Patellar Dislocation
Patellar dislocation refers to the knee cap (patella) dislocating from its usual location in the knee joint. Patellar instability refers to the knee cap being unstable where it usually resides. Recurrent patellar instability is a term often used to describe the situation where an athlete’s patella is dislocated multiple times over a period of time.
Causes patellar dislocation
A patellar dislocation occurs when a twisting injury to the knee joint causes the knee cap to dislocate. It usually occurs in sports when an athlete makes a plant and changes direction or performs a cutting motion. In doing so the foot remains firmly planted in the turf (or other playing surfaces) and the athlete’s body twists around his or her knee. As the quadriceps muscle (main thigh muscle in the front of the leg) contracts, the patellar is pulled out of its groove in the knee. Common sports where this can occur include football, soccer and basketball. Recently Mathew Stafford of the Detroit Lions dislocated his patella as did Chad Qualls, a pitcher for the Arizona Diamondbacks.
The patella is a free-floating bone in the front of the knee that is attached to the quadriceps muscle at the top and the patellar tendon at the bottom. On either side of the patella is a broad band of tissue, known as the retinaculum, that also has some stabilizing effect on the patella. The patella’s undersurface is shaped like a “V”, and it is covered with smooth articular cartilage. It glides within a groove at the end of the thigh bone (femur) that is called the trochlear groove. The trochlear groove is very important in maintaining the stability of the patella. How well developed and therefore deep the groove determines how much force it takes to dislocate the patella out of the groove.
The patella acts to transmit the force from the quadriceps muscles to the lower leg (tibia) through the patellar tendon. This mechanism straightens (extends) the knee joint. The patella, by moving the quadriceps away from the center of the knee, helps create more torque, and therefore power, by the quadriceps. This is very important because the quadriceps support all of someone’s bodyweight during walking and actually multiple times bodyweight during exercise and athletic activities.
Structures injured in a patellar dislocation
During a traumatic patellar dislocation, the ligament that normally guides the patella into its groove is torn. This 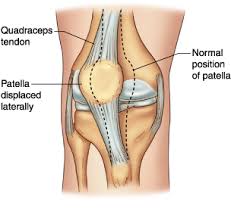 ligament is actually part of the patellar retinaculum on the inside of the knee and is known as the medial patellofemoral ligament (MPFL). As most patellar dislocations occur with the knee twisting near full extension, the patella at this point has not yet entered its groove which in most athlete’s knees keeps the patella very stable. It normally does so at about 20° of knee flexion, and up until this point the MPFL is the main structure responsible for keeping the patella centered in the knee. The patella in just about all cases dislocates towards the outside of the knee (lateral), therefore the medial ligament is injured as it stretches. The MPFL normally attaches to the patella on one end and the end of the thigh bone on the other end. It may be torn anywhere along its length from a dislocation.
ligament is actually part of the patellar retinaculum on the inside of the knee and is known as the medial patellofemoral ligament (MPFL). As most patellar dislocations occur with the knee twisting near full extension, the patella at this point has not yet entered its groove which in most athlete’s knees keeps the patella very stable. It normally does so at about 20° of knee flexion, and up until this point the MPFL is the main structure responsible for keeping the patella centered in the knee. The patella in just about all cases dislocates towards the outside of the knee (lateral), therefore the medial ligament is injured as it stretches. The MPFL normally attaches to the patella on one end and the end of the thigh bone on the other end. It may be torn anywhere along its length from a dislocation.
Associated injuries
As the athlete suffers a patellar dislocation there may be other injuries that occur within the knee joint itself. As the patella moves to the outside (lateral) the articular cartilage may be injured from a shearing mechanism. Rarely, a loose piece of cartilage can be knocked off either the end of the thigh bone (femur) or from the undersurface of the patella. This loose piece could potentially get caught inside the knee and produce catching and locking resulting in further damage inside the knee.
Risk factors
There are some factors that can predispose an athlete to a patellar dislocation. These factors can be classified as related to the knee itself or as factors not inherent to the knee. Factors related to the knee include poor bony development of the trochlear groove at the end of the thigh bone (femur) in which the patella normally glides. This is termed trochlear dysplasia and when present provides less than normal bony resistance to the patella dislocating. Another factor would be if the patella sits too high in the knee (patella alta). In this case the patella is further from the bony support of the trochlear groove and is more reliant on weaker soft-tissue ligaments to keep it centered in the knee. Lastly, if the attachment of the patellar tendon to the lower leg bone (tibial tubercle) is rotated too far to the outside, there is an inherent lateral (toward the outside of the knee) pull on the patella.
Factors not inherent to the knee itself include rotational malalignment to the leg which can involve the femur (femoral anteversion) or the tibia (tibial torsion). Both of these abnormalities align the thigh muscles to pull the patella more lateral than usual. Flat feet can also predispose to patella dislocations because the legs can become knock-kneed and again the pull of the thigh muscles is more lateral than usual. Furthermore if an athlete is very ligamentously lax (has loose ligaments and tendons), the ligaments holding the patella in place can stretch out more. Finally, weak core musculature and weak hip muscles can decrease the muscular control an athlete has over their entire lower extremity including the knees.
Diagnosis
In most cases, the athlete will describe a twisting episode where the knee cap dislocated and either reduced on its own or someone had to pop it back in place for them. Often an athletic trainer at the practice or event will witness the injury and help reduce the patella. Following the injury, the athlete will experience pain in the knee and usually considerable swelling. In some cases, the athlete will have experienced dislocations in the past. This is termed recurrent patellar instability and should be addressed differently than a first-time incident.
On examination if the patella is still not reduced, it will be palpable on the outside of the knee. In most cases it can be easily pushed back into place. On occasion, this may require sedation in an emergency room. Once the patella is reduced there will be tenderness, usually on the inside (medial) aspect of the knee where the torn MPFL is located. Pushing the patella towards the outside of the knee will illicit a painful reaction from the patient known as patellar apprehension. There will be swelling inside the joint (effusion) if the dislocation was within the past few weeks. Lastly, there may be tenderness along the joint line of the patella if there is a cartilage injury present as well.
In the situation of recurrent dislocations, the athlete should be checked for all of the predisposing factors noted above. For example the looseness of their ligaments should be evaluated. The rotational alignment of their lower extremities and feet should be checked. Their hip and core strength should be assessed as well. These are often surprisingly weak in many athletes, especially teenagers.
Imaging tests considered
Radiographs should always be obtained. They are important to document that the patella is reduced and no longer dislocated. Any associated fractures can be evaluated. Any tilting of the patella can also be seen. Lastly, the height of the patella can be assessed as can the depth of the trochlear groove.
An MRI can be obtained to evaluate the MPFL and determine where it is torn. The MRI can also give a detailed look at the cartilage surfaces and see any other injuries within the knee. A CT scan is important to determine the bony alignment of the lower extremity and plan any surgeries in the case of an athlete with multiple dislocations.
Treatment for Patellar dislocation
Most first-time patellar dislocations are treated without surgery. This will include a short period of immobilization which typically lasts 2 to 4 weeks. Following this, physical therapy is important to regain range of motion and to work on strength about the knee.
Additionally, a focused strengthening program is important for the athlete’s core and hip abductor muscles. This is important in prevention of a future dislocation.
Once the swelling of the knee is down and the athlete is pain free with full range of motion, they can begin sports-specific drills and eventually return to their sport.
The majority of athletes who dislocate their patella successfully return to their sport after a period of rehab. This may require a few months of steadily progressing physical therapy. Only a small handful, typically less than 20% have symptoms from recurrent patellar instability.
More Information: Read about sports injury treatment using the P.R.I.C.E. principle – Protection, Rest, Icing, Compression, Elevation.
Surgery
Even though most athletes do well without surgery, a small number of patients may do better off having surgery early on for their patellar dislocation. When there are loose pieces of bone or cartilage floating in the knee, these can get stuck and cause further damage. In this case an arthroscopy is useful to remove these loose bodies. If there is residual persistent tilting of the patella in a lateral direction once it is reduced, the MPFL may be too stretched to heal properly without repair.
Patellar dislocation surgery
When an athlete suffers a patellar dislocation on multiple occasions, they may wish to have their knee surgically corrected to avoid further instability episodes. Planning surgery for recurrent dislocations requires a complex work-up involving a careful physical exam to evaluate all the factors described above as well as obtaining advanced imaging studies. It is important to determine which anatomic factors are present and correct each of them surgically. For example if an athlete has a deficient MPFL as well as a tibial tubercle that is too far rotated, then both a repair or reconstruction of the MPFL is required along with a realignment procedure for the tibial tubercle. Therefore it is important that the athlete is evaluated by a highly trained sports medicine specialist who is experienced taking care of patellofemoral pain.
Surgical treatment options for a patellar dislocation
In the majority of cases it must be determined if the MPFL is deficient and also if the tibial tubercle is malrotated. If the MPFL is deficient it can be either repaired or reconstructed with a graft. A reconstruction where either an autograft (patient’s own tissue) or an allograft (cadaveric tissue) is used to create a new MPFL ligament may be necessary if the MPFL tear is longstanding and the tissue present is of poor quality to repair with sutures. If the tibial tubercle is rotated too much, then it can be cut (osteotomy) and reattached with screws at an improved location.
In the rare case where the groove for the patella (trochlear groove) is too shallow, then this may have to be addressed with surgery to make the groove deeper. In the similarly rare situation of a patella that sits too high on the knee, surgery may be required to bring the patella down to a more normal position so that it rides better in its groove.
Patellar dislocation surgery recovery
If arthroscopy is performed to remove loose bodies in the knee following a dislocation, then the recovery is relatively quick and not much different from non-operative treatment. Physical therapy will be necessary for a few months in order for the athlete to regain their range of motion and strength.
Patellar stabilizing surgery will take much longer for an athlete to recover from. These typically require a larger open incision. Following surgery, there will be a period of time where the ligament repair or reconstruction will have to heal. If a bone cut is performed for the tibial tubercle, then there will be a period of time necessary for the bones to heal together. Although there will be variability depending on the specific surgery performed, recovery from these procedures will commonly take many months.
Patient outcomes following surgery for patellar dislocations
Most athletes are able to recover following patellar stabilization procedures. However the results of surgery are not quite as reliable as seen following the more common torn meniscus or torn ACL surgeries. A patient must realize the amount of rehab necessary following surgery for patellar dislocations and that they may need to perform regular exercises to maintain good control over their hips and lower extremities to prevent future dislocations.
Can Telemedicine Help?
Telemedicine is gaining popularity because it can help bring you and the doctor together quicker and more efficiently. It is particularly well suited for sports injuries and facilitating the diagnoses and treatment of those injuries. Learn more about speaking with a sports specialized provider via SportsMD’s 24/7 Telemedicine Service.
Professional athletes with Patellar Dislocation:
Chicago SunBears inside linebacker Danny Trevathan is helped off the field after suffering a torn patellar tendon against the Titans on Nov. 27, 2016. (Charles Rex … Undaunted Danny Trevathan returns — ‘I’m looking to be even better … – Chicago Sun-Times
The 25-year-old Gervacio once played for the Tornadoes in the 2014 Grand Prix and 2015 All Filipino where she suffered a dislocated patella. The 5-foot-8 open spiker returned to action in the Shakey’s V League for BaliPure and Perlas in the PVL … Foton looking to recruit Gervacio – Inquirer.net
HARRISON HILL/NYT Bethanie Mattek-Sands positions herself before her rehab session at the Hospital for Special Surgery in New York, July 19, 2017. Mattek-Sands ruptured and dislocated her kneecap in a singles match at Wimbledon, but her disposition … An upbeat recovery after an injury that shook Wimbledon – MyAJ
References:
Patellar instability. Colvin AC, West RV. J Bone Joint Surg Am. 2008 Dec;90(12):2751-62.
The management of recurrent patellar dislocation. Andrish J. Orthop Clin North Am. 2008 Jul;39(3):313-27
The medial patellofemoral ligament. Dopirak RM, Steensen RN, Maurus PB. Orthopedics. 2008 Apr;31(4):331-8.
Outcomes of medial patellofemoral ligament reconstruction for patellar instability: a systematic review. Smith TO, Walker J, Russell N. Knee Surg Sports Traumatol Arthrosc. 2007 Nov;15(11):1301-14. Epub 2007 Aug 8.
Rehabilitation and nonoperative treatment of patellar instability. McConnell J. Sports Med Arthrosc. 2007 Jun;15(2):95-104.
Restoration of native medial patellofemoral ligament support after patella dislocation. Tom A, Fulkerson JP. Sports Med Arthrosc. 2007 Jun;15(2):68-71.

