Scaphoid Fracture Surgery
Last Updated on August 12, 2024 by The SportsMD Editors
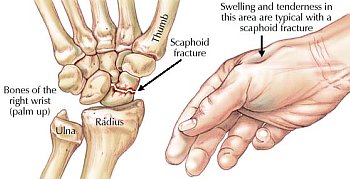
The scaphoid is a small bone in the wrist on the thumb side. The wrist is a complex joint that is composed of the end of the radius (the big bone in the forearm, on the thumb side), the ulna (the small bone in the forearm, on the small finger side) as well as the carpal bones. There are 8 carpal bones: the scaphoid, lunate, triquetrum, pisiform, hamate, capitate, trapezoid, and trapezium. These bones are connected by ligaments, making the wrist a fairly complex joint.
The scaphoid is the most commonly fractured wrist (“carpal”) bone. It is located in the thumb side of the wrist. If you put your thumb up in the air (like a hitchhiker) you will make a small depression at the base of your thumb. This depression is called the “anatomic snuffbox.” If you press with your finger deep into the floor of the anatomic snuffbox, you can barely feel the scaphoid. The scaphoid plays a critical role in maintaining the normal, pain-free motion of the wrist that is required with many athletic activities.
The scaphoid doesn’t have a great blood supply, which is one of the reasons that the scaphoid fracture sometimes doesn’t heal. Its blood supply comes mostly from the far (distal) end instead of the near (proximal) end. The scaphoid is shaped like a twisted peanut and is only about 1 inch long or a little shorter. Eighty percent of the scaphoid is covered with cartilage, such that most fractures of the scaphoid bone will extend into some joint.
A scaphoid fracture is a common, career-threatening wrist injury that has been seen in virtually every sport.
What is a scaphoid fracture?
A scaphoid fracture is any break or crack in the scaphoid. There are many different ways one can experience a scaphoid fracture, and the type of fracture may change how it is treated. Usually it results from either direct trauma to the wrist in contact athletes, or indirectly from a fall on an outstretched hand and wrist with other sports. There are several ways to describe a scaphoid fracture.
 They may be displaced or nondisplaced. If the fracture is nondisplaced, it is still perfectly lined up. These may be considered for treatment without surgery (with a cast). Most displaced fractures benefit from surgery. Surgery can allow better “reduction” or alignment of the fracture fragments into a normal position and can increase the rate of predictable healing of the fracture.
They may be displaced or nondisplaced. If the fracture is nondisplaced, it is still perfectly lined up. These may be considered for treatment without surgery (with a cast). Most displaced fractures benefit from surgery. Surgery can allow better “reduction” or alignment of the fracture fragments into a normal position and can increase the rate of predictable healing of the fracture.
A scaphoid fracture can also be described by the location. It may be at the far end (distal pole), in the middle (waist), or at the near end (proximal pole). The fractures at the near end (closer to the elbow, proximal pole) have a poorer blood supply and are less likely to heal without surgery. In addition, the “near end” (proximal pole) is at risk of dying (“avascular necrosis”) without prompt treatment.
Several other terms may be used to describe a scaphoid fracture. An acute fracture is one that is diagnosed soon after it happened. An occult fracture is one that is discovered long after it happened, and it may benefit from surgery.
A nonunion is a scaphoid fracture that still has not healed 6 months after it occurred. Nonunions of these fractures can be career threatening for athletes, and it is important that they seek the counsel of a hand and wrist surgery specialist to determine an appropriate treatment plan.
Diagnosis of scaphoid fracture
A scaphoid fracture may be suspected in an athlete that falls onto an outstretched hand and then has wrist pain. If the athlete has a scaphoid fracture, they will usually have tenderness in the anatomic snuffbox. They may also have pain with movement of the wrist and thumb and reduced grip strength.
If a scaphoid fracture is suspected, x-rays will be taken. These will show the fracture most of the time, but sometimes fractures will not show up on x-rays if it is a nondisplaced fracture. If a scaphoid fracture is suspected and the plain x-rays are not diagnostic, there are 3 main options. One option is to get an MRI. Another option is to get a bone scan. Another option is to cast the wrist as if there is a scaphoid fracture, then 2 weeks later re-examine the wrist and repeat x-rays. If there is a fracture, it should be visible on the x-rays taken 2 weeks after the injury.
If an athlete has a scaphoid fracture and it is difficult to tell on x-rays whether or not it is displaced, a CT scan may be ordered. This will show if there is any displacement and help with surgical planning.
If the athlete has a nonunion (a fracture that has not healed after 6 months), an MRI may be ordered to see whether the bone fragment still has a blood supply to help with surgical planning.
Causes of scaphoid fracture
Usually it happens due to a fall onto the outstretched hand with the wrist bent back (extended) and towards the thumb (radially deviated). However, it can also occur from direct trauma to the wrist in contact sports, such as with a tackle in football or check into the boards with hockey.
Non-surgical treatment
Initially, sports injury treatment using the P.R.I.C.E. principle – Protection, Rest, Icing, Compression, Elevation can be applied to a scaphoid fracture.
Treatment without surgery can be considered in athletes when the scaphoid fracture is nondisplaced (it is cracked but it is still perfectly lined up) and if it is not a fracture of the upper end (proximal pole fracture). If treatment without surgery is chosen, a cast is placed that includes the thumb, wrist, forearm, and possibly the elbow. Including the elbow causes less motion at the fracture site, and may increase healing rates. Often a cast that includes the elbow is used for the first 4-6 weeks, and then a cast that does not include the elbow is used for an additional 4- 6 weeks. Typically, the total time in a cast is 8-12 weeks, or possibly longer depending on how fast the bone heals. Return to sports depends on many factors and must be decided on an individual basis. If it is a noncontact sport, it may be reasonable to return to play immediately in the cast if compatible with the sport. If it is a contact sport, it is more controversial, but one reasonable option may be to have no contact for the first 6 weeks, then resume full contact play in the cast for the next 6 weeks. When nondisplaced fractures are treated appropriately in a cast, there is an 88-95% chance of healing if treatment is started within a couple of weeks after injury.
Even with minimally displaced fractures, however, many athletes will seek surgical fixation to avoid prolonged cast immobilization and allow controlled range-of-motion right away.
Scaphoid fracture surgery
Treatment with surgery is generally appropriate for any scaphoid fracture that is displaced more than 1 mm or any fracture at the upper end (proximal pole). Surgery may also be considered for nondisplaced fractures, to lessen the time of cast immobilization.
The reason for choosing surgery for displaced fractures and fractures of the upper end is that treating these fractures in a cast carries a 10-55% risk of delayed union (taking a long time to heal), nonunion (not healing at all), or losing the blood supply to a bone fragment (avascular necrosis or AVN). Also, if the fracture heals in the wrong position (“malunion”), it may lead to continued wrist pain, loss of motion, or eventual arthritis. Any or all of these complications can threaten an athletic career and limit the ability of the athlete to return to the previous level of competition.
The reasons for choosing surgery of a nondisplaced fracture are a little more controversial, because a cast will lead to healing most of the time. However, choosing surgery instead of casting alone may lead to faster healing and less time in a cast or splint. In the setting of a well-executed surgery, very high rates of predictable healing with a low risk of complications have been reported for minimally displaced fracture fixation.
Surgery is also appropriate for a scaphoid fracture that is discovered long after it occurred and for nonunions (fractures that have not healed after 6 months). The surgical plan is variable and depends on many factors, including fracture alignment, the status of the blood supply to the fragments, and previous treatments. Longstanding scaphoid nonunions have been associated with a predictable pattern of arthritic change and associated loss of motion that can threaten the careers of athletes in virtually every overhead or upper extremity sport.
What does scaphoid fracture surgery entail?
Surgery is usually an outpatient procedure (the athlete may go home the same day of surgery). Depending on the fracture type, there may be an incision on the front or back of the wrist which is used to access the scaphoid to line up the fracture and place a metal screw to hold it in place.
If the scaphoid fracture is a nonunion it may be necessary to place some bone graft as well, which may be taken from the radius (by the wrist), the iliac crest (by the hip), or from a cadaver. If one of the bone fragments has lost its blood supply, a vascularized bone graft (graft with its own blood supply) may be considered. This is when a small piece of bone from the radius with its very small blood vessel is moved into the fracture site to give it a blood supply.
What are the complications of surgery?
The complication rate is low, but there is the potential for infection, nerve injury, stiffness, problems with the hardware, or failure of the bone to heal.
Scaphoid fracture recovery
After scaphoid fracture surgery, a splint or cast is typically applied, and then 1-2 weeks later, this may be changed to a removable brace or another cast may be used depending on the fracture type and competing sport. Return to sport must be individualized based on the type of scaphoid fracture recovery and what sports the athlete is involved in, so it may vary substantially between athletes. If the athlete is involved in noncontact sports, it may be reasonable to go back to sport 1-2 weeks after surgery with a brace or cast to protect the wrist. If the athlete is involved in contact sports, it may be reasonable to return to play in a cast 3-6 weeks after surgery, but there is some degree of risk involved with that decision. When the cast is removed, rehabilitation involves gentle range-of-motion and strengthening of the wrist. This is individualized based on the injury and surgery so it is important that the athlete discuss this with their physician and follow their directions. Often, a CT scan is taken to document healing of the bone before activities are allowed without a brace or cast. It is typically 3 months or longer before it is healed sufficiently to allow for sports without a brace or cast. Sports that demand significant wrist motion, like tennis or hockey, may require complete healing and pain-free, full range-of-motion before successful return to play is achieved.
Get a Virtual Sports Specialized appointment within 5 minutes for $29
 When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
References:
- Adams JE, Steinman SP. Acute scaphoid fractures. Orthop Clin N Am 2007;38:229-35.
- Gutow AP. Percutaneous fixation of scaphoid fractures. J Am Acad Orthop Surg 2007;15(8):474-85.
- Kawamura K, Chung KC. Treatment of scaphoid fractures and nonunions. J Hand Surg 2008;33A:988-97.
- Kovacic J, Bergfeld J. Return to play issues in upper extremity injuries. Clin J Sports Med 2005;15(6):448-52.
- Waitayawinyo T, McCallister WV, Nemechek NM, Trumble TE. Scaphoid nonunion. J Am Acad Orthop Surg 2007;15:308-320.

