Bennett’s fracture
Last Updated on October 22, 2023 by The SportsMD Editors
Five bones (“metacarpals”) are in the hand that connect the bones of the wrist (“carpus”) with those of the digits (“phalanges”). Approximately ¼ of metacarpal fractures occur in the thumb metacarpal. Of these fractures of the thumb metacarpal, 80% occur at the base (the end closer to the wrist). The Bennett’s fracture is the most common type of fracture to the thumb metacarpal base. A Bennett’s fracture is an intra-articular fracture, or one that extends into the joint between the metacarpal and wrist bone (“trapezium”). This injury most often occurs in contact sports such as football, rugby, and boxing.
Why is it called a Bennett’s fracture?
In 1882, Edward Hallaran Bennett, M.D., an Irish surgeon, described five cases of an “intra-articular” fracture dislocation. He went on to suggest that despite the relatively benign appearance of the fracture, prompt recognition and treatment is necessary to preserve function of this complex, highly mobile joint. Because of Dr. Bennett’s early work on this injury, the fracture is still commonly known as a Bennett’s fracture.
Anatomy involved in a Bennett’s fracture
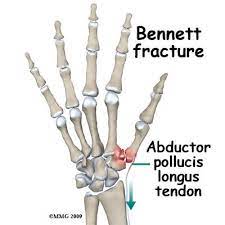
The Bennett’s fracture occurs at the base of the thumb metacarpal (the longest bone in the thumb) where it articulates with one of the carpal (wrist) bones called the trapezium. It forms the thumb or first carpometacarpal (CMC) joint. The contour of the trapezium and thumb metacarpal base forms a saddle-joint and contributes significantly to the joint’s stability. This creates a complex joint that allows the thumb to have complex motion and to function as an opposable digit. In a Bennett’s fracture, the fracture begins at the volar (palm side), ulnar base of the thumb metacarpal and extends in an oblique fashion distally. The volar oblique ligament connects the base of the thumb with the trapezium and is the primary soft-tissue stabilizer of the thumb CMC joint. This strong ligament functionally remains intact after a Bennett’s fracture and allows the articular fracture fragment to maintain its anatomic relationship with the trapezium. However, the rest of the metacarpal fragment is subject to deforming forces that create a tendency toward further fracture displacement. The distal fragment is displaced proximally, radial (towards the thumb side), and dorsal (behind the rest of the hand) by the pull of the abductor pollicus longus (APL) muscle. Furthermore, the adductor pollicus (ADP) attaches near the metacarpal head and pulls the distal fragment towards the palm.
Diagnosis
 The typical presentation is seen in an athlete with a recent history of an axial load to a flexed thumb such as a fall onto an outstretched hand. Athletes will have pain and swelling noted at the base of the thumb. Active motion is limited because of pain. Once appropriate suspicion for a fracture is present, standard posteroanterior, lateral, and oblique radiographs (x-rays) should be obtained. Additionally, a “prayer” view may provide a more focused view of the thumb metacarpal joint as well. If plain films still do not provide adequate evaluation of the fracture, CT scans can be obtained of the affected area. Your treating physician will not only take careful note of the size and displacement of the fracture fragment, but also will evaluate for the presence of cartilage injury (the smooth tissue that lines the joint surfaces) on both the metacarpal and trapezium.
The typical presentation is seen in an athlete with a recent history of an axial load to a flexed thumb such as a fall onto an outstretched hand. Athletes will have pain and swelling noted at the base of the thumb. Active motion is limited because of pain. Once appropriate suspicion for a fracture is present, standard posteroanterior, lateral, and oblique radiographs (x-rays) should be obtained. Additionally, a “prayer” view may provide a more focused view of the thumb metacarpal joint as well. If plain films still do not provide adequate evaluation of the fracture, CT scans can be obtained of the affected area. Your treating physician will not only take careful note of the size and displacement of the fracture fragment, but also will evaluate for the presence of cartilage injury (the smooth tissue that lines the joint surfaces) on both the metacarpal and trapezium.
Causes
The classic mechanism for injury that produces a Bennett fracture is an axially directed force (force applied to the end) of a partially flexed thumb metacarpal. This injury mechanism can be seen in boxing but is also commonly seen in sports such as football or rugby. Injury is most commonly seen in the dominant hand (2/3) and predominates in men at nearly a 10:1 ratio.
Bennett’s Fracture Treatment
Since Dr. Bennett first described the fracture that bears his name, many authors have advocated for different methods of Bennett’s Fracture treatment. Much of the past scientific data on treatment is conflicting. There is certainly no uniform consensus on what initial fracture treatment results in the best long term outcome. Closed reduction (manipulation) and cast immobilization often leads to satisfactory short-term results without significant functional impairment. However, because of the extension of this fracture into the joint and the significant deforming forces from muscles, worsening fracture step-off and displacement is often seen with closed treatment methods. This is typically poorly tolerated by high level athletes, particularly in the dominant hand. If an adequate closed reduction is achieved, cast treatment may be a reasonable option provided the fracture is carefully followed and that the reduction (“good alignment of the bones”) can be maintained.
Some of the more recent literature looking at long-term follow-up has suggested that surgical treatment to restore near perfect or perfect alignment of the bones (“anatomic reduction”) results in lower rates of arthritis. Unfortunately, the correlation is not clear in the literature between radiographic arthritic changes and severity of symptoms or need for future operations to address symptomatic thumb arthritis.
More Information: Read about sports injury treatment using the P.R.I.C.E. principle – Protection, Rest, Icing, Compression, Elevation.
Bennett’s Fracture Surgery options
Treatment and surgical decision making regarding a Bennett’s fracture should be undertaken by an orthopaedic surgeon or a hand surgery specialist who has experience with treating these injuries. When dealing with athletes, it is important for the surgeon to be familiar with the unique demands of the athlete. If it is determined that surgery is appropriate, the surgeon will usually align the bone fragments and use either pins or screws to hold the fracture in place. If the fracture can be reduced without making an incision, often two pins will be placed through poke holes and cut just below the skin. If the surgeon needs to make an incision to “line up” the fracture fragments, either K-wires or screws can be placed through the incision to hold the fracture fragments in place. If wires are used, they can typically be removed after the fracture shows signs of healing, usually at 4 to 6 weeks after surgery. In the athlete, especially the high level athlete, surgical intervention is more effective in stabilizing the fracture and often allows for an earlier return to sport.
Get a Telehealth Appointment or Second Opinion With a World-Renowned Orthopedic Doctor
 Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
Will I need to wear a cast for Bennett’s Fracture?
If surgery is not needed, a short forearm cast that includes the thumb called a thumb spica cast is typically worn for 6 weeks. If surgery is elected, often for the first 4-6 weeks a thumb spica cast or a thumb spica splint is worn at all times to protect the fracture fragment position until healing occurs. However, each fracture severity and pattern is different. For this reason, the stability of the fracture fixation and the specific requirements of an athlete’s sport has to be carefully considered to create an individualized plan for splinting or casting.
When can I return to sports?
To answer this question, many factors have to be considered. First, the stability of the fracture after surgical treatment or nonoperative treatment has to be determined. For example, if a large fracture fragment was solidly repaired with multiple screws, the surgeon may have confidence releasing an athlete to activity sooner. In the same way, the level of athletic participation needs to be considered. The type of sporting activity also is an important factor in determining return to play. Bennett fractures are commonly seen as football injuries. If an NFL offensive lineman has a Bennett’s fracture in the non-dominant hand and is surgically treated, he may be able to return to competitive play in 4 weeks and play with a padded cast or splint in place. If this same fracture occurred in the dominant hand of a quarterback, his time out of competitive play would be significantly longer. This is because the activity of accurately throwing a football requires more function from the thumb CMC joint and wearing a cast/splint is ineffective. Ultimately, the decision on when to return to sports should be determined on a case-by-case basis after careful evaluation by the treating surgeon and athlete.
Question and Answers:
When discussing Bennett’s fracture or any medical condition with a doctor, it’s important to ask questions to fully understand your situation and treatment options. Here are some questions you can ask, along with potential answers from a healthcare professional:
- What is a Bennett’s fracture?
- A Bennett’s fracture is a specific type of fracture at the base of the thumb, typically involving the first metacarpal bone.
- How did I get this fracture, and what are the common causes?
- Bennett’s fractures are often caused by direct trauma to the thumb, such as a forceful impact or a fall.
- What are my treatment options?
- Treatment options may include conservative management with a splint, cast, or surgical intervention, depending on the severity of the fracture.
- What are the potential risks and benefits of surgery?
- Surgery can provide more stable and precise alignment of the fractured bone, but it also involves potential risks, such as infection or complications with anesthesia.
- How long will my recovery take?
- Recovery time varies depending on the treatment method and the severity of the fracture. It’s important to discuss the expected timeline for your specific case.
- What signs of complications should I watch for during recovery?
- Be sure to ask about warning signs of complications, such as infection, and when to seek medical attention.
- Do I need a follow-up appointment, and when should it be scheduled?
- Establish a plan for post-treatment follow-up appointments to monitor your progress.
Remember that your doctor will tailor their responses to your specific case, so feel free to ask any additional questions or seek clarification on any points you don’t fully understand. Open and honest communication with your healthcare provider is essential for your treatment and recovery.
References:
- Atkison R, Athletic Injuries of the Hand, in DeLee JC, Drez D, Miller MD (eds): DeLee and Drez’s Orthopaedic Sports Medicine, 3rd ed. Missouri: WB Saunders, 2009.
- Bennett EH. On fracture of the metacarpal bone of the thumb. BMJ 1886; 2:12-13.
- Soyer AD. Fractures of the Base of the First Metacarpal: Current Treatment Options. JAAOS 1999; 7(6): 403-412.

