Distal Biceps Tendon Rupture
Last Updated on August 12, 2024 by The SportsMD Editors
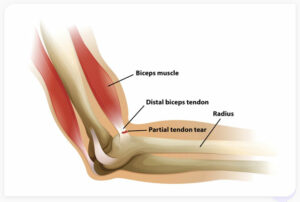
The biceps muscle is an important muscle in the upper arm. As its name implies, the “bi-ceps” has two origins around the shoulder (one within the shoulder joint, and the other from the shoulder blade at the “coracoid process”) that join the muscle belly as it courses along the front of the upper arm to insert in the proximal forearm (“radius” bone). The distal tendon of the biceps muscle transmits all of the forces of the muscle to the radius at its insertion (“radial or bicipital tuberosity”), thereby contributing to an athlete’s ability to forcefully flex at the elbow as well as rotate their forearm in turning the palm upward (“supination”). The distal biceps tendon is therefore subject to very high forces in attaching the muscle to bone, and can also be injured with repetitive microtrauma in athletes.
What is a distal biceps tendon rupture?
The distal biceps tendon rupture is a tear of the biceps tendon that prevents the transmission of forces from the muscle to the forearm bones. While it can happen from repetitive injury in athletes, it more commonly results from a single traumatic event in which the flexed elbow is resisted or even traumatically extended. The event is usually accompanied by a “popping sensation” and a sense of sharp tearing around the elbow crease. A distal biceps tendon rupture has an equal effect on the dominant and nondominant arms of athletes. Fortunately, these injuries are relatively uncommon, occurring in 1 to 2 per 100,000 people. Furthermore, they are rarely seen in female athletes. The reason for this gender difference remains unclear.
In most cases, the distal biceps tendon rupture are complete tears, such that there is no connection between the muscle and the bone. Partial tears can occur, however, in which the tendon is not fully detached and can still be palpated at the elbow flexion crease. In the case of a partial injury, the loss of strength is usually less pronounced.
Consequences of a distal biceps rupture in an athlete
Once a distal biceps tendon rupture occurs, it unfortunately will not heal on its own. Rather, the tendon will continue to retract away from the bone and slide up the arm as the muscle contracts without resistance. Over time, the tendon will become stiff and scarred as well. This loss of biceps muscle function is mostly commonly manifest by an approximately 30% loss of elbow flexion strength and 40% loss of forearm rotation strength (specifically turning the palm “upward”) in the arm. While this may be tolerated in low-demand patients and perhaps in the nondominant arm of an athlete, most athletes will be impaired by the weakness without a surgical repair. In young patients with a dominant arm injury, these injuries should typically be addressed acutely with surgical repair.
What puts me at risk as an athlete for a distal biceps tendon rupture?
A distal biceps tendon rupture usually occurs when the flexed elbow is traumatically forced straight. This can certainly occur in contact sports such as football, hockey, lacrosse, and rugby. However, it can also occur in recreational athletes or weightlifters or attempt to lift more weight than can be handled, resulting in traumatic tearing of the tendon as the arm is gradually extended. While this unfortunate event can affect virtually every athlete, some factors that have been associated with a greater risk for distal biceps tendon rupture include:
• Male
• ≥ 30 years of age
• “Weekend Warrior” athlete – generally, a lack of regular stretching and conditioning predisposes tendons and their insertions on bone to traumatic injury with athletic activity.
• Smoking
• Corticosteroids – both systemic and local injections can weaken tendons.
• Certain antibiotics – the quinolone family of antibiotics (“-floxacins”) have been shown to adversely affect tendon biology and may increase risk of traumatic injury.
Symptoms of distal biceps tendon rupture
 Usually, the presentation of a distal biceps tendon is not subtle in the athlete. There will be the acute onset of a “tearing sensation” at the elbow, often accompanied by a “pop” when the tendon ruptures off the bone. When compared to the normal arm, the tendon can no longer be palpated at the elbow flexion crease. Frequently, there is swelling and bruising around the elbow flexion crease as well. The athlete will have significant weakness with flexion and twisting of the forearm (“supination”) with an evident loss of fullness in the front of the elbow. Over the next few days after injury, a bulge from the retracted muscle and tendon can develop in the upper arm – a so-called “Popeye” sign of biceps tendon injury.
Usually, the presentation of a distal biceps tendon is not subtle in the athlete. There will be the acute onset of a “tearing sensation” at the elbow, often accompanied by a “pop” when the tendon ruptures off the bone. When compared to the normal arm, the tendon can no longer be palpated at the elbow flexion crease. Frequently, there is swelling and bruising around the elbow flexion crease as well. The athlete will have significant weakness with flexion and twisting of the forearm (“supination”) with an evident loss of fullness in the front of the elbow. Over the next few days after injury, a bulge from the retracted muscle and tendon can develop in the upper arm – a so-called “Popeye” sign of biceps tendon injury.
The diagnosis of a distal biceps tendon rupture can usually be made based on the straightforward physical exam findings and history of injury.
Imaging Tests for biceps tendon rupture
In addition to the physical examination, your doctor might suggest imaging tests to help confirm a diagnosis. An imaging study is often useful to confirm the injury, determine the location of tearing, and measure the degree of tendon retraction. Occasionally, the tendon itself can tear at the muscle-tendon junction rather than detaching from the bone. In these cases, surgical repair is often less successful.
Furthermore, a significantly retracted tendon in a chronic or missed injury is important to recognize, as a primary repair to bone may no longer be possible in this setting. Both ultrasonography (US) and magnetic resonance imaging (MRI) can provide this important information.
X-rays: While X-rays can’t reveal soft tissues like the biceps tendon, they can be helpful in ruling out other conditions that could be causing your elbow pain.
Ultrasound: This imaging method is capable of showing the loose end of the biceps tendon that has retracted within the arm.
Magnetic resonance imaging (MRI): MRI scans provide more detailed images of soft tissues compared to X-rays. They can display both partial and complete tears in the biceps tendon.
Nonsurgical treatment
Most distal biceps tendon ruptures in active athletes should be addressed with surgical repair, particularly those in the dominant arm. The tendon should be repaired within 2 weeks of the injury. Tendon scarring and retraction with a delay beyond 2 weeks may limit the ability to primarily repair the tendon back to bone. While conduit “donor” tendons (“allograft”) from cadavers can be used in this setting to bridge the gap, the outcome is generally less successful with regards to restoration of strength in athletes.
Nonoperative treatment is not unreasonable in elderly or low-demand patients who rupture their biceps tendon, particularly when it has occurred in a non-dominant arm. In this setting, the patient may not be impaired or even notice the loss of flexion and supination strength from the injury. In addition, patients with missed injuries or those who seek delayed treatment may have chronic or “irreparable” tendon ruptures in which the outcome of a surgical repair may not be significantly better than nonoperative management. Other arm muscles can substitute for the ruptured biceps tendon and can provide full motion and reasonable function. High-level athletes, particularly overhead athletes, however, will usually appreciate the strength deficit.
Distal biceps tendon rupture surgery
Distal biceps tendon ruptures are usually treated with surgical repair of the tendon to bone within 2 weeks of the injury. Various techniques can be used by treating surgeons to achieve this result, ranging from simple drill holes to small implants (“anchors”) with sutures that help to attach the tendon to bone. The specific technique is probably less important as long as the tendon is apposed to the bone securely during the healing process. One incision or two incision approaches to repair the biceps tendon have been described. Each approach has its risks and benefits, such that selection is probably best guided by the surgeon’s expertise after a discussion with the athlete.
Delayed or missed injuries are more difficult to manage. The scarring and severity of retraction of the tendon usually help to guide treatment in these circumstances. Surgical repair with or without a “conduit graft” may be pursued if it is felt that direct or indirect apposition of the tendon to bone is feasible. Return of strength, however, is less predictable in this setting and risk of surgical complications is greater due to the more extensive dissection and exposure.
The exposure and repair of a ruptured distal biceps tendon can be performed safely, but is not without risk of complications even in the “best of hands.” A number of critical nerves and blood vessels reside in the area of the tendon insertion. The estimated complication rate is between 6% to 10%. These include:
• Sensory or motor nerve injury from retraction near the tendon insertion on the “radial tuberosity”
• Extra bone formation (“heterotopic ossification”) from trauma and exposure of the bone
• Recurrent rupture
• Infection
• Blood vessel injury
Rehabilitation after distal biceps repair
The arm is usually protected in a splint or brace in a flexed position after surgery until the surgical wounds heal. Gentle, passive motion of the arm is usually initiated soon in a protected setting. The process is gradual as the tendon-bone interface must be protected during the healing process. Resistance exercises are subsequently added to the rehabilitation plan after full motion of the elbow and forearm is achieved.
While light activities can resume soon after surgery, a full return to sports (particularly contact or lifting sports) can typically be anticipated no earlier than 3 to 4 months after surgery to allow the tendon to securely heal to bone. For heavy lifting or “full contact” positions in football or rugby, it may be advisable to wait 6 months. While the process is gradual, the outcome is usually successful with a predictable return to play with full strength and function.
Get a Virtual Sports Specialized appointment within 5 minutes for $29
 When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
Questions and Answers
When discussing a distal biceps tendon rupture with a healthcare provider, it’s essential to ask questions to fully understand your condition and potential treatment options. Here are some questions you can ask, along with potential answers:
- What is a distal biceps tendon rupture?
- A distal biceps tendon rupture is when the tendon that connects the biceps muscle to the elbow is partially or completely torn.
- What caused my distal biceps tendon rupture?
- Common causes include sudden, forceful arm movements, lifting heavy objects, or chronic overuse.
- How was the rupture diagnosed in my case?
- Diagnosis often involves a physical examination, medical history, and imaging studies like ultrasound or MRI.
- What symptoms should I expect with a distal biceps tendon rupture?
- Symptoms may include pain, weakness, bruising, and a bulge in the upper forearm.
- Is treatment necessary for a distal biceps tendon rupture?
- Treatment depends on the severity of the rupture and the patient’s activity level. Some cases may require surgical repair, while others can be managed conservatively.
- What are the treatment options for a distal biceps tendon rupture?
- Treatment options include surgical reattachment of the tendon or non-surgical management, such as physical therapy and modified activity.
- How long will the recovery process take, and what can I expect during this time?
- Recovery time varies depending on the treatment approach, but it typically takes several months. Rehabilitation and physical therapy are usually needed.
- What restrictions or limitations should I expect during the recovery period?
- Your doctor will explain any limitations on activities to protect the healing tendon.
- What are the potential complications associated with treatment and recovery?
- Complications can include infection (for surgery), stiffness, and strength deficits. Your doctor can discuss these in detail.
- Do I need a follow-up appointment, and when should it be scheduled?
- Establish a plan for post-treatment follow-up appointments to monitor your progress and make any necessary adjustments to your care.
Always consult with your healthcare provider for personalized answers to these questions, and feel free to ask additional questions or seek clarification on any points you don’t fully understand. Effective communication with your doctor is crucial for your understanding and overall care.
References
Vishwanathan, K., & Soni, K. (2021). Distal biceps rupture: Evaluation and management. Journal of Clinical Orthopaedics and Trauma, 19, 132–138. doi:10.1016/j.jcot.2021.05.012

