Os Acromiale
Last Updated on August 12, 2024 by The SportsMD Editors
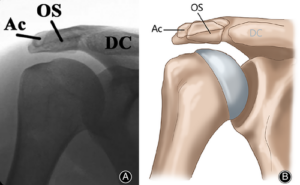
The acromion is part of the scapula or shoulder blade that extends laterally over the shoulder joint. When one of the four ossification centers or growth plates of the acromion fails to fuse, an os acromiale forms. While most os acromiale do not cause any symptoms, a few can severely limit a patient’s shoulder function because of pain.
Who is at risk for developing an os acromiale?
Studies have shown that about 8% of the population have an os acromiale. Of the patients with an os acromiale, 30-60 % of them will have them on both sides. Os acromiale are more commonly found in blacks and males than whites and females.
Causes of os acromiale
The acromion develops from four ossification centers or growth plates. The growth plates generally fuse by age 18 but can fuse as late as age 25. When there is failure of the growth plates to fuse an os acromiale develops. Failure of fusion can occur at any of the ossification centers but more commonly occurs anteriorly or in the front of the acromion.
Symptoms for os acromiale
 Most people who have an os acromiale do not have any problems. It is usually discovered when looking at the shoulder for another reason. Patients with symptomatic os acromiale can have pain with overhead activity. The pain will be located along the superior aspect of the shoulder. Symptoms can also occur at night. Along with pain, patients may have decreased shoulder motion and strength. Patients will be tender to palpation at the site of the os acromiale and there may also be frank movement of the bone at the site.
Most people who have an os acromiale do not have any problems. It is usually discovered when looking at the shoulder for another reason. Patients with symptomatic os acromiale can have pain with overhead activity. The pain will be located along the superior aspect of the shoulder. Symptoms can also occur at night. Along with pain, patients may have decreased shoulder motion and strength. Patients will be tender to palpation at the site of the os acromiale and there may also be frank movement of the bone at the site.
How does an os acromiale cause pain?
An os acromiale can cause pain in two ways. First, there can be pain from the movement of the unfused bones. The movement of the bone from the pull of the shoulder muscles can also pinch the soft tissue within the shoulder. This impingement can irritate the muscles, tendons, and bursa (fluid filled sac between muscles and bones) resulting in pain with shoulder movement. Patients can also get impingement within the shoulder from other sources though and be asymptomatic from their os acromiale.
Diagnose for os acromiale
A patient’s history of symptoms and findings on a physical exam can help the doctor make the diagnosis. X-rays will show the nonunion of the acromion. An MRI will also show the os acromiale along with other structures within the shoulder. The MRI may help differentiate the source of the pain.
the diagnosis. X-rays will show the nonunion of the acromion. An MRI will also show the os acromiale along with other structures within the shoulder. The MRI may help differentiate the source of the pain.
Nonsurgical treatment options for os acromiale
Patients who do not have symptoms from their os acromiale do not require any treatment. For symptomatic os acromiale, the first goal of treatment is to reduce inflamation and pain relief.
There are several home remedies that can help alleviate OS Acromiale, such as P.R.I.C.E Treatment:
- Protection: The purpose of protection is to avoid further injury to the area by protecting the injured structures. The type of protection used varies depending on the injured area but may include an ace bandage, aluminum splint, sling, protective tape, or over-the-counter brace.
- Rest: The purpose of resting is to allow the body’s own healing processes to naturally occur without being impeded by movement of the injured area. Any increase in movement of an injured tissue results in increased circulation to the area which in turn may result in further damage to the injured tissue and/or increased swelling.
- Ice: Ideally, ice packs are made of crushed ice because the crushed ice is more comfortable for the athletes and conforms to the contours of the injured area better than cubed ice. Ice can be placed into plastic or Ziploc bags. A light barrier should be placed between the skin and the ice bag (paper towel) to prevent injury to the skin during the application of the ice.
The ice pack can be secured with an ace bandage if needed. The ice should be applied for 20 minutes at a time and then removed. This can be repeated every two hours while the athlete is awake.
- Compression: When the ice pack is removed, a compression wrap should be applied to the injured area. The compression wrap serves as a mechanical barrier so that swelling is minimized in the injured area. There are a number of compression wraps available on the market, but the most commonly used is an elastic or ace bandage.
- Elevation: Elevation is important immediately post-injury to reduce the amount of blood flow to the injured area. For the lower extremities, the athlete can elevate his/her leg by lying down and elevating the injured limb on pillows. The key is that the athlete needs to have the injured area above his/her heart level.
Following the PRICE principles is an effective way to minimize the swelling in an injured area so that the athlete can return to play quickly.
Non-steroid anti-inflammatory drugs (NSAIDs) like Motrin®, ibuprofen, or Aleve® can help with pain control and decrease inflammation. Activities that cause symptoms should be avoided.
A physical therapy program that focuses on establishing non-painful shoulder motion and strengthening of the shoulder muscles will also be helpful. Selective injection within the nonunion site or in the subacromial space (between the acromion and shoulder joint) may provide pain relief and will also help differentiate the source of the patient’s pain.
How long should I try nonsurgical treatments for os acromiale?
It is recommended to continue non-operative treatments for os acromiale for at least 6 months unless the patient has other conditions like a torn rotator cuff that may require earlier surgical intervention.
Surgical treatment options for os acromiale
There are three main options available for the treatment of os acromiale. Surgical treatment options are based on the size and location of the os acromiale, the patient’s symptoms, age, and functional demands.
Small fragments located in the anterior or front of the acromion can be surgically removed. Patient’s who fail more extensive procedures may also require excision of the fragment as a salvage procedure. Removal of larger fragments though, may impair the function of shoulder’s deltoid muscle. This in turn may limit the shoulder’s function.
Larger fragments may require fixation with screws and wires along with bone graft (usually taken from the patient’s hip) in order to get the two fragments to fuse. A second surgery may be required to remove the hardware if they irritate the patient. It generally takes 9-12 weeks for the bone to heal. There is always the risk that the bone does not heal though.
A third option is to debride the undersurface of the acromion and the bursa to help with pain relief. There are minimal risks with this procedure but results may be mixed with persistent pain.
Get a Virtual Sports Specialized appointment within 5 minutes for $29
 When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
Os acromiale (blue). Secondary ossification center of acromion usually fuses by age 25, if persists without bony fusion = Os acromiale. Best seen on axial images, prevalence 1-15%. Usually asymptomatic, may be associated with shoulder impingement and rotator cuff tear. #FOAMrad pic.twitter.com/4YrGTMNt23
— Daniel J. Kowal, MD | Radiologist Headquarters (@RadiologistHQ) December 9, 2022
Question and Answers
When discussing Os Acromiale or any medical condition with a doctor, asking questions can help you better understand your situation and treatment options. Here are some questions you can ask, along with potential answers from a healthcare professional:
- What is Os Acromiale?
- Os Acromiale is a condition in which the acromion, a part of the shoulder blade (scapula), fails to fully fuse during development, resulting in a separate bone segment.
- What are the common causes of Os Acromiale?
- Os Acromiale is usually congenital, meaning it’s present from birth, and occurs as a result of the incomplete fusion of different acromion growth centers.
- How was Os Acromiale diagnosed in my case?
- Your doctor likely identified Os Acromiale through a physical examination, X-rays, or other imaging studies.
- What symptoms should I expect with Os Acromiale?
- Os Acromiale can cause shoulder pain, weakness, or discomfort. Your doctor can provide more information based on your specific case.
- Is treatment necessary for Os Acromiale?
- Treatment depends on the severity of your symptoms. Some cases may require conservative management, while others may benefit from surgical intervention.
- What are the treatment options for Os Acromiale?
- Treatment options may include physical therapy, pain management, or surgery to fuse the separate bone fragments. Your doctor will discuss the best approach for you.
- How long will the recovery process take, and what can I expect during this time?
- Recovery time varies depending on the chosen treatment method and the individual. Your doctor can provide an estimate based on your specific case.
- What is the long-term outlook for Os Acromiale?
- Your doctor can provide information about the expected long-term effects and whether you can anticipate a full recovery.
- Do I need a follow-up appointment, and when should it be scheduled?
- Establish a plan for post-treatment follow-up appointments to monitor your progress and adjust the treatment plan as needed.
Always consult with your healthcare provider for personalized answers to these questions, and feel free to ask additional questions or seek clarification on any points you don’t fully understand. Effective communication with your doctor is essential for your understanding and overall care.
References
- Hutchinson, M. R., and Veenstra, M. A. Arthroscopic decompression of shoulder impingement secondary to os acromiale. Arthroscopy,9: 28-32, 1993
- Kurtz CA, Humble BJ, Rodosky MW, Sekiya JK. Symptomatic Os Acromiale. Journal of the American Academy of Orthopaedic Surgeons 2006; 14:12-19
- Phillips, BB. “Arthroscopy of the Upper Extremity.” Campbell’s Operative Orthopaedics 11th Edition. Canale, ST, Beaty JH. Philadelphia: Mosby, 2008. 2966
- Vanderbeck JL et al. “Congenital Anomalies and Variational Anatomy of the Shoulder.” The Shoulder 4th Edition. Rockwwod Jr. CA et al. Philadelphia: Saunders, 2009. 122-124
- Warner JJ, Beim GM, Higgins L. The treatment of symptomatic os acromiale. J Bone Joint Surg Am 1998;80: 1320-1326.

