Patellar tendon rupture
By Bryson P. Lesniak, MD and Asheesh Bedi, MD
Last Updated on August 12, 2024 by The SportsMD Editors
Patellar tendon rupture is a rupture of the tendon that connects the patella to the tibia. The patellar tendon is the terminal extension of the quadriceps muscle in the leg. The four muscles that make up the quadriceps each provide a tendon that attaches to the kneecap (patella). The patella essentially lies within the quadriceps tendon and is therefore called a “sesamoid” bone. The quadriceps tendon becomes thicker and narrower as it travels from the kneecap to the shin bone (tibia). This thicker and somewhat narrower tendon is called the patellar tendon because it starts at the patella and ends at the tibia.

The patellar tendon is instrumental in allowing a person to straighten his/her leg. When the quadriceps contracts the force is transmitted through the quadriceps tendon and the patellar tendon, using the patella as a fulcrum and thus straightening the leg. If any link in this chain is disrupted- whether through a quadriceps tendon rupture or the patellar tendon rupture, a patella fracture or inability to contract the quadriceps muscle- the leg cannot extend at the knee. Keith Grennan of the Cleveland Browns, Cadillac Williams of the Tampa Bay Buccaneers, Kelenna Azubuike of the Golden State Warriors, and Correll Buckhalter of the Denver Broncos have all suffered from a patellar tendon rupture.
Athletes at risk for a patellar tendon rupture
A patellar tendon rupture tends to occur in people age 40 and younger. After the approximate age of 40 years, the quadriceps tendon becomes the more common tear in the extensor mechanism. Any condition that affects the quality or integrity of tendons or ligaments increases the risk of rupture; for example, diabetics and patients who take corticosteroids for an extended period of time for diseases like systemic lupus or rheumatoid arthritis. A growing population at risk is athletes that take anabolic steroids to increase their performance. Steroids can weaken the tendon and increase the risk of its rupture.
Symptoms of Patellar tendon rupture
An athlete that has a patellar tendon rupture has immediate pain and swelling in the knee area. He or she will often say they felt a “rip” or “tear” sensation and will be unable to ambulate because of weakness and pain. On examination, there are several tell-tale features in addition to pain and swelling in the knee. First, the athlete will be unable to actively straighten the leg. In addition, the examiner can usually palpate a defect in the tendon below the kneecap. However, in some cases the swelling in the knee joint (knee effusion) is severe enough that this is difficult to appreciate. The knee effusion in combination with severe pain with motion often requires radiologic examination to assist in making the diagnosis.
Patellar tendon tear MRI
Knee X-rays are the first imaging studies that are obtained and can be very helpful. When the patellar tendon ruptures, the patella shifts superiorly because of muscle contraction of the quadriceps muscles. This shift in the patella position is called “patella alta.” X-rays also evaluate the knee for any other injuries that can present similarly to a patellar tendon rupture such as a fracture. If any doubt remains after physical examination and X-rays, an ultrasound or magnetic resonance imaging (MRI) can be performed.
Ultrasonography is a safe, inexpensive and rapid test that can detect a tendon tear. However, the test is technician dependent and in some facilities is not a reliable diagnostic test. MRI is also a safe test but is more expensive and takes longer to perform. In addition, availability of MRI’s can be limited in emergency rooms and a doctor’s office. However, an MRI can also evaluate any other potential problems in the knee such as ligament or cartilage injury.
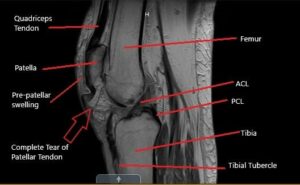
In the vast majority of athletes who have suffered a patellar tendon rupture, an MRI is not indicated as the diagnosis is made with X-rays and physical examination. However, in the case of partial tears, chronic tears or an unusual presentation, an MRI can be a useful diagnostic tool.
Causes patellar tendon rupture
It is generally accepted that healthy, “normal” patellar tendons do not rupture. That is, there is an underlying degeneration in the tendon prior to complete rupture. The usual circumstance surrounding a patellar tendon rupture is when a person suddenly contracts the quadriceps muscle when the knee is in a flexed position. A common example is running up a flight of stairs or when a running backstops running quickly to change direction.
Patellar tendon surgery
For an athlete, patellar tendon surgery is often recommended. If the tear is treated non-operatively, athletes rarely have the ability to extend the leg and ambulate normally without assistance.
Patellar tendon rupture surgery, while not an emergency, should be performed soon after the injury occurred. This allows for an easier repair before a significant accumulation of scar tissue. Most surgeons perform a direct repair of the tendon if it is torn in the middle. If the tendon is torn off of the bone, several different techniques can be utilized such as reattaching the tendon to the bone with a combination of sutures and bone tunnels. Regardless of technique, the goal of surgical repair is to re-approximate the tendon ends in a secure fashion to allow them to heal.
If the patellar tendon is not repaired soon after the injury (within 5-6 weeks), surgical repair can become more difficult and have suboptimal results.
If the tendon cannot be repaired back to itself, a reconstruction can be performed with a graft from donor tissue (allograft) or tissue taken from another part of the patient’s body (autograft).
Get a Virtual Sports Specialized appointment within 5 minutes for $29
 When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
Patellar tendon rupture recovery time
Patellar tendon rupture recovery time after surgery varies based on surgeon preferences. After surgery, athletes are placed in a patellar tendon rupture knee brace that keeps their knees straight. Most rehabilitation plans allow initiation of active knee flexion and passive extension by two weeks after surgery. At 6 weeks after surgery, athletes can walk without crutches. The stiffness that comes with the patellar tendon recovery, combined with muscle atrophy creates problems for athletes who need to place significant load through their knee. So early motion combined with early muscle activation is very important. Usually, a return to athletic activities is delayed until 4-6 months after surgery based on leg strength and range of motion. The rehabilitation for chronic reconstructions is more substantial and prolonged than above.
Results of surgical repair
If the repair is done acutely (within 3 weeks), most athletes report good or excellent results. Most athletes are able to return to their previous level of competition and do not report residual weakness or discomfort. The results with repairs done after 3 weeks are not as favorable because of persistent weakness or poor range of motion as the likely cause of disability.
Surgery complications
Loss of knee motion and quadriceps weakness are the two most common problems after surgery. Whether this is due to the initial injury or the surgical repair is difficult to determine, but likely due to the initial injury. With postoperative physical therapy as discussed above, the goal is to minimize these problems. Less common complications include persistent knee effusion, infection, and re-rupture of the repaired tendon.
References.
1. Siwek CW, Rao JP: Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am 1981; 63:932-937.
2. Larsen E, Lund PM: Ruptures of the extensor mechanism of the knee joint: Clinical results and patellofemoral articulation. Clin Orthop 1986; 213: 150-153.
3. Yu JS, Petersilge C, Sartoris DJ: MR imaging of injuries of the extensor mechanism of the knee. Radiographics 1994; 14: 541-551.
4. Ecker ML, Lotke PA, Glazer RM: Late reconstruction of the patellar tendon. J Bone Joint Surg Am 1979; 61:884-886.

