Birth Control and the Female Athlete
Choice of birth control method for the adult female athlete is as individual a choice as it is for any other woman. However, the female athlete, particularly if she is a high-level competitor, must consider additional factors when choosing a contraceptive method. This article will review the factors for consideration and how they relate to female athletes, but, as with any female patient, the final choice of the “best” method is left to the individual. The role of this article is to provide the female athlete with some of the general information she needs to make an informed decision.
What is the menstrual cycle?
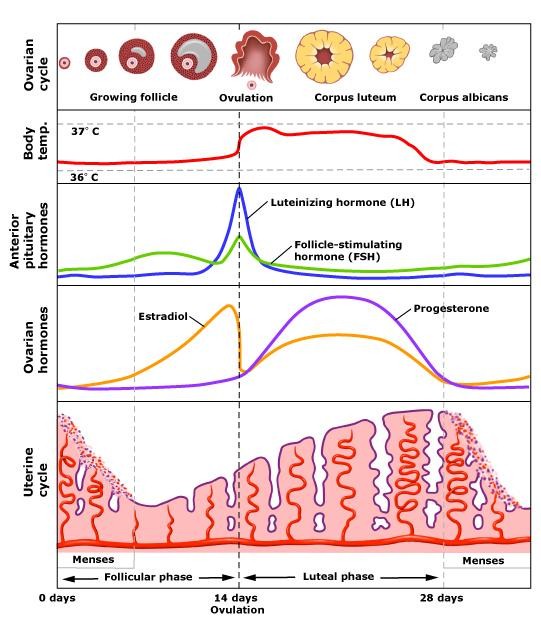
The menstrual cycle is the sequence of hormonal and physiological changes that take place in a woman’s body from the start of one period to the start of the next. Usually, the menstrual cycle is between 28-30 days, but some women have either longer or shorter cycles. Day 1 of the cycle is the day menstrual bleeding starts, and the last day is the day the next period’s bleeding starts.
Four hormones regulate the sequence of events in a cycle: follicle stimulating hormone (FSH), leutinizing hormone (LH), estrogen and progesterone. These split the cycle up into three phases: follicular phase (from start of menstrual bleeding to ovulation), ovulation, and the luteal phase (from ovulation to the start of the next bleed).
Follicle Stimulating Hormone (FSH) starts the whole process off at the beginning of the cycle. It is a hormone produced by the pituitary gland, a small stalked structure at the base of the brain. FSH does what it says – it stimulates follicles – the structures in the ovaries that house eggs – to stimulate the egg to mature to the point at which it is ready to be fertilized. The follicle and egg are “ripe” at about mid-cycle, usually 14 days after the start of the last period. Just before this point, a spike in the level of estrogen, a hormone produced by the ovaries, followed by a spike in the levels of LH and FSH from the pituitary, cause the ripe follicle to complete its maturation process and rupture in a process called ovulation. The estrogen and progesterone also help to stimulate the development and growth of the uterine lining. The ripened egg then floats away from the ovary and down the fallopian tube to the uterus. At any point of this journey, which usually takes a few days, it can be fertilized by a single spermatozoa. When a fertilized egg implants in the developed uterine lining, a pregnancy results. In the meantime, the ruptured follicle (“corpus luteum”) continues to produce progesterone and estrogen to stabilize the lining of the uterus in preparation for implantation of the fertilized egg. If a fertilized egg implants, the placenta, a vascular structure that nourishes the embryo, maintains the production of estrogen and progesterone. If an egg is not successfully fertilized and/or implanted, estrogen and progesterone levels decrease, causing the uterine lining to slough off in the menstrual bleeding that starts a new cycle.
How do hormones and the menstrual cycle affect athletic performance?
As any woman can tell you, periods can be a real pain, literally and figuratively. Bleeding is a hassle, requiring the use of tampons and sanitary napkins, and many women will experience some degree of menstrual cramping as the uterus expels blood and tissue. Some women are almost completely incapacitated by their periods, either due to intense cramping, heavy bleeding or both. In female athletes, monthly periods can interfere with exercise and training schedules. Some may feel slower, more sluggish, bloated, constipated and more easily fatigued during menstruation. It is difficult, if not impossible, to say how many of these feelings are truly physiologic and how many are due to social and psychological perceptions of menstruation. Nevertheless, the hormones that regulate the reproductive system also have effects on other organ systems and metabolic processes.
Estrogens:
Estrogens are a group of steroid hormones produced largely by the ovaries. They can be transformed into male sex hormones (“androgens”) in fat and muscle tissue. Along with their effects on the menstrual cycle, they also affect:
– the cardiovascular system by changing blood clotting mechanisms which can increase the chances of blood clot formation, and by dilating blood vessels.
– the musculoskeletal and hepatic (Liver) Systems by changing the metabolic balance of carbohydrates and fats, increasing the use of fats to preserve stored carbohydrate, changes which can also increase resistance to insulin resulting in higher blood sugar levels.
– The kidneys by causing retention of salt leading to swelling (“edema”), weight gain, and increased blood pressure.
– The skeletal system by increasing calcium uptake into bone and by building and maintaining bone density.
Progestins:
Progestins are a group of steroid hormones which have androgenic and anti-estrogenic activities. These include:
– increasing body temperature
– increased amoung of breathing (“minute ventilation”), the lungs’ reaction to decreased oxygen in the blood or increased carbon dioxide, potentially leading to a feeling of shortness of breath
– change the kidneys’ retention of salt and water leading to bloating and weight gain
All of these changes in physiology can certainly have an indirect impact on athletic performance. However, the direct effects of these changes in hormonal levels during the menstrual cycle on athletic performance remains unclear. Studies lead to conflicting conclusions because of different protocols and the use of subjective instead of objective data (i.e. they often rely on how the athlete thinks she is performing as opposed to objective results). Those that have measured hormone levels for objective timing of cycle phases often use different methods of measuring hormone levels. Nonetheless, the aspects of athletic performance that MAY be affected by hormonal cycle changes include:
– Decreased hemoglobin concentrations during menstruation that may lead to increased ventilation (i.e. a faster breathing rate)
– Salt and fluid retention as well as dilation of blood vessels that may decrease the blood flow rate through muscle, possibly resulting in suboptimal muscle function
– Changes in the lungs’ ability to process gas exchange as efficiently around menstruation that may lead to increased oxygen demand and an increased sensation of shortness of breath
– Increase in basal body temperature during the luteal phase that may increase the likelihood of heat-related illness in long endurance events (e.g. marathons) at higher ambient temperatures
– Metabolic changes, particulary during luteal phase, when blood lactate (a product of glucose breakdown in anaerobic activity) may decrease compared to during the follicular phase, leading to increased endurance.
– Some studies have suggested that women are more susceptible to ACL rupture during the ovulatory phase of the cycle as there are estrogen and progesterone receptors in the ACL
Other issues related to menstruation may affect athletic performance as well.
– Women with heavy periods are more likely to become “anemic” due to iron deficiency and blood loss (inability of the body’s iron stores to keep pace with blood loss), which can lead to shortness of breath, fatigue, light headedness and palpitations, all of which will impair performance
– Women with painful periods are less likely to perform well during their periods due to cramping
Why do female athletes sometimes have irregular periods?
A common issue for high-level female athletes is the absence of a menstrual cycle. This is often because they are expending more calories than they are taking in. This caloric stress is hypothesized to cause a disruption in the hormonal cycle starting at a region in the brain that controls the hormonal cycling in the pituitary and ovaries (“hypothalamus”). This disrupts the entire menstrual cycle so the woman no longer ovulates, indicating that the body is less able to nourish a fetus. It can also be secondary to high intensity of exercise or even the psychological stresses of competition. When women stop ovulating, their hormone cycle becomes more or less dormant and they lose some of the benefits of these hormones. The most obvious of these effects is the effect on bone metabolism. Amenorrheic women (women who are no longer ovulating or having menstrual cycles) are more at risk for osteopenia and osteoporosis, setting them up for stress fractures which can take them out of competition for weeks or months at a time.
How does birth control work and affect this process?
Broadly speaking, there are two categories of birth control: hormonal and non-hormonal. Hormonal methods include the Pill, the Patch, the NuvaRing, the Mirena IUD, Depo-Provera and Implanon. Non-hormonal methods include the copper intrauterine device (IUD), condoms, cervical caps, diaphragms, femidoms, and spermicidal gels and foams. Female athletes who use a hormonal form of contraception usually are effectively shutting down their normal hormonal cycles. Exogenous progestins and estrogens from the contraceptive effectively tell the pituitary not to produce FSH or LH and thereby suppress ovulation. They can also alter the thickness of the uterine lining, reducing the likelihood of a successful implantation of a fertilized egg.
How do the hormones from contraceptives affect athletic performance?
The simple answer is that no one really knows. A few small studies have evaluated the efficiency of oxygen utilization in exercise in women on “the Pill” versus matched controls. These have shown a small but significant decrease in oxygen utilization efficiency in women on “the Pill.” However, the study size was small and the percentage to which oxygen utilization was reduced was also small, in the order of 2-4%, a reduction which would most likely not be noticeable in recreational athletes but may potentially affect elite athletes.
Should female athletes use hormonal contraception?
The answer to this question remains unknown. Female athletes who suffer with heavy or painful periods may find that the psychological benefit they get from the decreased blood loss and pain improves performance. Women in competitive sports may also appreciate that ability to delay onset of menstrual bleeding to allow them to not be menstruating during important competitions. However, there are contraindications to using hormonal birth control methods in athletes at all levels. These include personal history of blood clots or history of blood clots in first degree relatives, known disorders in blood clotting, poor liver function, breast cancer, history of heart attack, high blood pressure, smoking, migraine headaches, or recent surgery.
Unfortunately, for those looking for definitive answers, there seem to be a lot more questions than answers in this particular area. What can be said with certainty is that there is no solid evidence that hormonal contraception decreases athletic performance and that many elite female athletes use hormonal contraceptives with no apparent deleterious effects. However, each athlete, indeed each woman, should examine the different birth control options she has and decide based on her own criteria, demands, and a thorough discussion with their treating physician.
Virtual Care from Sports Doctors and Specialists
 SportsMD offers Virtual Care and Second Opinion Services. It allows you to quickly and conveniently speak with a sports doctor or specialist and have an effective alternative to emergency room, urgent care, or waiting for a doctors appointment. You can get Virtual Care from your home or anywhere via phone or video chat.
SportsMD offers Virtual Care and Second Opinion Services. It allows you to quickly and conveniently speak with a sports doctor or specialist and have an effective alternative to emergency room, urgent care, or waiting for a doctors appointment. You can get Virtual Care from your home or anywhere via phone or video chat.
References:
- C M Lebrun, M A Petit, D C McKenzie, J E Taunton, J C Prior. Decreased maximal aerobic capacity with use of a triphasic oral contraceptive in highly active women: a randomised controlled trial. Br J Sports Med 2003;37:315–320
- Schelkun PH. Exercise and “The Pill”: Putting a Rumor to Rest. Phys Sportsmed. 1991 Mar; 19(3): 143-152
- Frankovich RJ, Lebrun CM. Menstrual Cycle, Contraception, and Performance. Clin Sports Med 2000 Apr; 19 (2): 251-71 4) Lebrun CM. The Effect of the Phase of the Menstrual Cycle and the Birth Control Pill on Athletic Performance. Clin Sports Med 1994 Apr; 13(2): 419-21.
- Quadagno D, Faquin L, Lim GN, Kuminka W, Moffatt R. The Menstrual Cycle: Does it Affect Athletic Performance? Phys Sportsmed 1991 Mar; 19 (3): 121-124.