Scapholunate Ligament Tear
Last Updated on August 12, 2024 by The SportsMD Editors
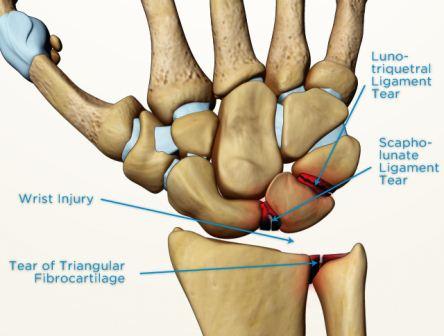
Although there are many ligaments and injuries in the wrist, a scapholunate ligament tear is the most commonly injured. The scapholunate ligament connects the scaphoid to the lunate. The most important part of the ligament is on the back (dorsal side) of the wrist. Normally, the scaphoid and the lunate move together because the scapholunate ligament connects them tightly. When a scapholunate ligament tear occurs, the scaphoid bends forward (flexes) and the lunate bends backwards (extends) and a gap may form between the bones.
The wrist is a complex joint that is composed of the end of the radius (the big bone in the forearm, on the thumb side), the ulna (the small bone in the forearm, on the small finger side) as well as the carpal bones. There are 8 carpal bones: the scaphoid, lunate, triquetrum, pisiform, hamate, capitate, trapezoid, and trapezium. These bones are all connected by ligaments, making the wrist a very complex joint which is actually a collection of multiple joints.
The scaphoid is a small bone in the wrist on the thumb side. It is located in the thumb side of the wrist. If you put your thumb up in the air (like a hitchhiker) you will make a small depression at the base of your thumb. This depression is called the “anatomic snuffbox.” If you press with your finger deep into the floor of the anatomic snuffbox, you can barely feel the scaphoid. The scaphoid is shaped like a twisted peanut and is only about 1 inch long or a little shorter. 80% of it is covered with cartilage.
The lunate is a small bone in the center of the wrist right next to the scaphoid. It is shaped like a crescent moon when viewed from the side.
What is a scapholunate ligament tear in athletes?
A scapholunate ligament tear can vary from mild sprains (partial tears or “stretches”) all the way to complete tears with other torn ligaments. They may also be accompanied by other injuries such as a scaphoid fracture or a lunate dislocation. These are more severe injuries, and for the purpose of this article, we will still stay focused on the scapholunate ligament tear.
One way to think about the scapholunate ligament tear is to divide them into four categories in order from mild to severe: predynamic, dynamic, static, and scapholunate advanced collapse.
Predynamic, or occult, injury is the mildest form of the scapholunate ligament tear. It is a partial tear of the ligament. X-rays are normal, but the partial tear may be visualized by an MRI or by looking in the joint with an arthroscope at the time of surgery.
In a dynamic injury, the ligament is completely torn or stretched to the point that it can’t do its job. There may also be some mild injury to other surrounding ligaments. Regular x-rays are normal but stress x-rays show a gap between the scaphoid and the lunate (see next section below “How is a scapholunate ligament tear diagnosed?” for discussion regarding stress x-rays.)
In a static injury, the ligament is completely torn, and some of the surrounding ligaments are also injured. Regular x-rays show a gap between the scaphoid and the lunate.
In a scapholunate advanced collapse (SLAC) injury, the ligament is completely torn, and the injury has been there a long time (years) causing arthritis, or evidence of cartilage damage, to be seen on regular x-rays in addition to the gapping between the scaphoid and the lunate. This is a predictable pattern of arthritis that develops with longstanding, untreated ligament injuries.
Injuries may also be classified according to how long it has been since the injury: Acute (less than 4 weeks), subacute (4 weeks to 6 months), and chronic (more than 6 months).
Scapholunate ligament tear diagnosis
A scapholunate ligament tear is usually caused by a fall or by a sudden load on the wrist. Sometimes the athlete may not recall the fall because they didn’t seek treatment immediately, but instead sought treatment weeks later when they continued to have pain. The athlete may have pain in the center or on the thumb side of the wrist, especially with activities such as push-ups, or other activities that load the wrist. There may also be grip weakness, snapping, swelling, or popping.
When the physician examines the athlete, the scapholunate interval may be tender and swollen. The Watson scaphoid shift test can be helpful. This is done by bending the wrist toward the small finger. Then the physician applies pressure to the palm side of the scaphoid as the wrist is bent toward the thumb. Relief of pressure will allow the scaphoid to slip back into place with a clunk. However, this test may be positive in many normal wrists, so it must be interpreted with caution and compared to the other side.
There are several imaging studies that may be used: standard x-rays, stress x-rays, and scapholunate ligament MRI. Standard x-rays rule out other problems such as fractures. If the athlete has a static injury (see “What is a scapholunate tear?” in the above section), the standard x-rays will show gapping between the lunate and scaphoid and increased angulation between the scaphoid and the lunate. If the athlete has a longstanding tear with a SLAC wrist, arthritis may be seen on the x-rays.
If standard x-rays are normal, stress x-rays may be useful to see gapping or instability that is too mild to show up on standard x-rays. To perform stress x-rays, the athlete simple makes a tight fist for one x-ray, then bends the wrist forcefully towards the small finger for another x-ray, then bends the wrist towards the thumb for another. The physician may also order an x-ray during which your fingers are gently pulled on. These x-rays may show gapping or abnormal angulation that only occurs during activities, but not when the wrist is at rest. Sometimes, x-rays of the normal wrist may be taken for comparison.
Depending on the situation, MRI may be useful. This may be ordered as an MRI arthrogram, which means the radiologist will inject dye into the wrist with a needle before the MRI. If there is a tear or a hole in a ligament, the dye will leak through. However, MRI’s and arthrograms are not 100% accurate. Sometimes an MRI may miss an injury because the ligament is so small and sometimes the dye will leak through even if there is not a ligament injury. That is why your physician will take into account your symptoms, history, exam, and x-rays rather than just relying on a MRI alone to come up with the best treatment plan.
Scapholunate ligament tear. Increased distance between scaphoid and lunate. pic.twitter.com/eQlu3yHDat
— Stefan Tigges (@StefanTigges) April 16, 2019
If the diagnosis is still unclear, or if it is clear that surgery is needed, arthroscopy (looking inside the wrist with a camera at surgery) may be used to clearly define the injury. Arthroscopy is the most accurate way to define the scapholunate ligament tear, but it is a surgery.
Treatment for a Scapholunate ligament tear
Treatment without surgery may be appropriate in a predynamic injury, or a mild sprain of the scapholunate ligament without changes on x-rays. This may involve a wrist brace or a cast for 2-6 weeks, minimizing activity that causes pain such a tight gripping or pushing, and anti-inflammatory medications such as ibuprofen. Then a removable brace may be used for activities, as gradual strengthening and stretching is added. Return to sports depends on the severity of the symptoms and the type of sport as well as if the athlete can participate in the sport with a cast or brace.
If this is not successful, surgery such as wrist arthroscopy may be considered. Based on what is found at the time of arthroscopy, the ligament may be debrided (“cleaned up”) or pins may be placed with a cast.
P.R.IC.E Treatment
Mild sprains can be treated with P.R.I.C.E.
Protection. The purpose of protection is to avoid further injury to the area by protecting the injured structures. The type of protection used varies depending on the injured area but may include an ace bandage, aluminum splint, sling, protective tape, or over-the-counter brace.
Rest. Avoiding activities that put a lot of stress on your wrist is crucial to promote healing and prevent complications. If you have to use your wrist or hand, you can use a wrist brace, which is shown to improve pain and confidence. Besides, you may use an over-the-counter pain medication to reduce pain and inflammation.
Ice. Ice can help reduce pain and swelling, as it numbs the affected wrist and decreases blood flow to the area. Apply ice—wrapped in a damp towel— to the wrist for 15 minutes at a time, 3 to 4 times a day.
Compression. Wrap the wrist with an elastic bandage or a compression wrap to reduce swelling and support your wrist. Avoid compressing too tightly. Doing so can impair circulation to the area. If the compressed area feels numb or tingly, loosen the bandage.
Elevation. Keep the injured wrist above the level of the heart as often as possible. To do so, try lying down with a pillow on your chest and rest your wrist on the pillow.
When to See the Doctor
Hundreds of athletes sustain acute injuries everyday, which can be treated safely at home using the P.R.I.C.E. principle. But if there are signs or symptoms of a serious injury, emergency first aid should be provided while keeping the athlete calm and still until emergency service personnel arrive. Signs of an emergency situation when you should seek care and doctor treatment can include:
- Bone or joint that is clearly deformed or broken
- Severe swelling and/or pain,
- Unsteady breathing or pulse
- Disorientation or confusion
- Paralysis, tingling, or numbness
In addition, an athlete should seek medical care if acute symptoms do not go away after rest and home treatment using the P.R.I.C.E principle.

Scapholunate Ligament Tear Surgery
If there is gapping and increased angulation between the scaphoid and lunate on x-rays, or if treatment without surgery hasn’t been successful, then surgery is warranted.
If the x-rays don’t show gapping, but treatment with a cast or brace has not been successful, arthroscopy is an option. This involves placing a camera in the wrist to examine the injury. Based on what is found, the joint may be debrided (“cleaned up”). If significant instability is found, pins may be placed to hold the bones in place and/or an incision may be made to repair or reconstruct the ligaments.
If x-rays show gapping, as in dynamic or static injuries, then surgery is warranted. This involves repairing the ligament. The ligament repair may be augmented by tightening up the capsule tissue on the back of the wrist. Then pins are usually placed to help protect the ligament repair while it is healing.
Scapholunate ligament recovery time
The first 1 to 2 weeks after surgery
- After surgery, a splint is placed which is then changed to a cast at 1-2 weeks. The cast protects the repair as well as the pins, which are protruding through the skin.
2 to 8 weeks after surgery
- Initiate range of motion and continue to protect the wrist
- Still no weight bearing activities
2 to 3 months after surgery
- The pins and cast are removed
- Patient will use a removable wrist splint to provide support and protect the wrist
- Hand therapy and home exercises are initiated
3 months to 5 months and beyond
- Start strengthening wrist exercises lead by your physical therapists starting with 1-2 lbs. weights and progressively increasing to 10 lbs. from 3 to 5 months. At 5 months a return to gentle exercises and to sport at 5 to 6 months after surgery and when cleared by your doctor to play. A wrist brace may be recommended during this period, even for low-impact activities.
When can I return to play after surgery?
Return to sport depends on the athlete’s exact injury, surgery, and sport. The athlete should discuss this with their physician. Certainly, leg work and the well arm may be used throughout the recovery process. Return to contact sports may be considered after pin removal with a removable protective brace. Return to contact sports without a brace may be considered at 6 months.
When might surgery fail?
If x-rays show gapping and arthritis, then ligament repair is not likely to work. In that case, treatment without surgery may be tried because surgical options are more involved and may involve removing some wrist bones or causing some bone to grow together (fusion). In this situation, treatment without surgery may involve bracing, anti-inflammatory medications, avoiding painful activities, and cortisone injections.
Have questions about your wrist pain? Speak to Sports Specialized Provider within minutes for $29.
 How severe is your injury? Do I need to see a doctor or can this be managed at home? What should be my treatment plan? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365. Learn more via SportsMD’s Virtual Urgent Care Service.
How severe is your injury? Do I need to see a doctor or can this be managed at home? What should be my treatment plan? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365. Learn more via SportsMD’s Virtual Urgent Care Service.
References:
- Kuo CE, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg 2008;33A:998-1013.
- Lewis DM, Osterman AL. Scapholunate instability in athletes. Clin Sports Med 2001;20(1):131-40.
- Manuel J, Moran SL. The diagnosis and treatment of scapholunate instability. Orthop Clin N Am 2007;38:261-77.
- Walsh JJ, Berger RA, Cooney WP. Current status of scapholunate interosseous ligament injuries. J Am Acad Orthop Surg 2002;10:32-42