How to Treat Tendonitis
Early intervention is the key in how to treat tendonitis. Tendonitis can be successfully treated but it is important to note that the treatment protocol for tendonitis is unique and different than treating other acute injuries. The wrong treatment can exacerbate the condition increasing the time for recovery and getting back to sport.
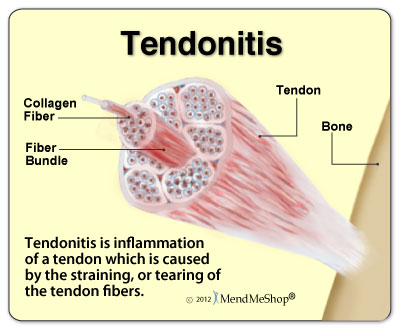
Tendonitis can affect many body segments. Although the body segments may differ, the structural damage and healing process are the same. Understanding the basic structure and function of a tendon will give the athlete a better understanding of why the treatment protocol for tendonitis is different than other types of acute injuries.
What is the structure and function of a tendon?
The purpose of a tendon is to connect muscle to bone. While the specific structure of a tendon may vary from tendon to tendon, the components are the same. A tendon is primarily made up of collagen fibers, water, and ground substance. It is the components in the ground substance that give the tendon its viscoelastic properties (ability to stretch and return to its original shape).
In a resting state, a tendon has a wavy appearance. When the muscle attached to the tendon contracts, the tendon straightens out and becomes tighter.
Some tendons are wrapped in synovial sheaths (achilles and biceps tendons). In tendons where a sheath is present, the blood supply for the tendon comes primarily from the synovial sheath. The synovial sheath also contains a very small amount of fluid to help reduce friction between the tendon and sheath while the tendon elongates.
As with muscle tissue, a tendon has a structural breaking point. Initially, when stress is applied to the tendon, the tendon will elongate. If the force continues beyond what the tensile strength of the tendon can handle, the tendon will eventually rupture.
What are the classifications of tendonitis?
There are six classifications of tendonitis ranging from mild to severe. Each classification is based on the amount of pain the athlete experiences before, during, and after exercise and is correlated to the athlete’s functional ability.
Mild tendonitis (levels 1 and 2) is usually associated with pain with extreme exertion that stops when activity stops. The athlete can usually continue to compete with mild tendonitis without any functional impact to his/her ability to perform.
Moderate tendonitis (levels 3 and 4) is usually associated with pain with extreme exertion that lasts several hours after the activity. Moderate tendonitis may begin to affect the athlete’s ability to perform at high levels. As the inflammation increases towards level 4, the athlete’s ability to perform at a normal level may begin to be impacted.
Severe tendonitis (levels 5 and 6) is usually associated with pain during the activity that may continue to last throughout the day and night. The athlete may also have pain in the affected region during everyday activities and not just during athletic performance.
What causes tendonitis?
Tendonitis is considered an overuse injury caused by repetitive loading of a tendon exceeding the ability of the tendon to handle the load. Repetitive loading of a tendon can breakdown otherwise normal tissue resulting in pain, swelling, and decreased functional ability of the associated joint.
Common causes of tendonitis include the following:
• Excessive increases in training load, distances, and speed
• Mechanical errors from improper technique
• Structural abnormalities
• Inappropriate equipment, play or work conditions
• Training surfaces (surfaces that do not give)
• Muscle imbalances
• Inadequate time for tendon recovery
What happens to the structure of the tendon when it is overloaded?
The initial response of the tendon is inflammation. In fact, when you break down the word tendonitis, “itis” means inflammation. Add “itis” to tendon and you have inflammation of a tendon.
Initially, the tendon becomes painful to the touch and begins to weaken. If the tendon is continuously overloaded, the tissue begins to break down.
A number of structural changes can occur during this process including thickening of the synovial sheath surrounding the tendon, areas of abnormal tissue known as fibrosis are laid down within the tendon, thickening of connective tissue, and adhesions (scar tissue laid down in and around the tendon). The longer the condition goes untreated, the more structural changes occur.
How to treat tendonitis? – First Step
The first step in how to treat tendonitis is to identify the cause. This step cannot be overemphasized because even if you treat the tendonitis, the condition will return if the cause has not been identified and dealt with.
Identifying the possible causes of tendonitis begins with a detailed history of the athlete specifically looking at specific load increases. These may include significant increases in the amount of activity (number of repetitions), distance (mileage) increases, and/or speed increases.
For example, in a softball pitcher suffering from bicipital tendonitis in her throwing shoulder, one would specifically look at the number of pitches thrown, the types of pitches thrown, the distances of pitches thrown, and the intensity of pitches thrown. If there was an identifiable jump in the number, type, distance, or intensity of pitches thrown that triggered the tendonitis, then the therapist can work with the coach to reduce the workout to one in which the athlete can compete safely and without damage to her tendon.
If there is not an obvious increase in the athlete’s history that triggered the tendonitis, an analysis of the athlete’s mechanics may be in order. If the sports medicine professional is not proficient in the athlete’s sport, the professional may need to consult with the athlete’s coach.
In order to ensure that the tendonitis does not return, the causative factors must be identified and changed prior to the athlete returning to sport.
How to treat tendonitis
The initial phase in how to treat tendonitis is to get the inflammation under control. If the tendon is acutely inflamed (tender to the touch, swollen, and painful with movement), the treatment needs to focus on reducing the inflammation.
Acute inflammation can be treated using the P.R.I.C.E. principle of Protection, Rest, Ice, Compression, and Elevation with the focus on rest and ice. Rest is absolutely crucial in treating tendonitis and is the most difficult component to get an athlete to adhere to. However, athletes who continue to push through pain risk moving their injury from the acute inflammation phase to a chronic tendonitis which is much harder to treat.
Once again, the longer an athlete plays with tendonitis, the more structural changes and damage there will be to the tendon. As the tendon worsens, the time frame for healing the tendon significantly increases.
If complete rest from the activity is not possible, the athlete needs to accommodate his/her activities to reduce the amount of stress on the tendon. For example, the softball pitcher with bicipital tendonitis can perform wrist work for ball rotation rather than full arm rotation pitches. The pitcher can also reduce the number and intensity of pitches thrown focusing more on mechanics than speed.
When trying to reduce inflammation in a tendonitis, the initial treatment focus is not on exercises, but on calming down the inflamed tendon. This is the key difference between treating a sprain or a strain versus treating tendonitis. While traditional rehabilitation protocols for most acute injuries focus on increasing range of motion and strengthening the surrounding muscles, tendons, and ligaments, initial treatment for tendonitis focuses on reducing inflammation.
Early exercise for an individual with tendonitis can make the condition worse. The patient will have an increase in pain and swelling the day after treatment rather than a reduction in symptoms. This is one way to tell if the treatment is too aggressive.
During early tendonitis treatment, the sports medicine professional may also prescribe anti-inflammatory medication to help reduce the inflammation. Rest, ice, and anti-inflammatory medications are the primary treatment protocol during early rehabilitation for tendonitis.
Get a Telehealth Appointment or Second Opinion With a World-Renowned Orthopedic Doctor
 Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
When can I proceed to range of motion and strengthening exercises?
As pain and swelling dissipate, the athlete can then move carefully into a progression of exercises to improve the range of motion of the affected tendon and strengthen the tendon. However, because of the delicate nature of the tendon, these exercises need to be carefully monitored to ensure that the athlete does not digress in his/her symptoms.
Flexibility exercises should focus on gradually elongating the tendon without causing an increase in pain. If fibrosis or adhesions are noted in the tendon by the sports medicine professional, he/she may apply one or more soft tissue techniques to help release the adhesions that may be interfering with the tendon’s ability to elongate.
Strengthening exercises should focus on light intensity and higher repetitions so as not to place too much stress on the tendon. Research has also supported the use of eccentric strength exercises (lengthening contraction) early in the rehabilitation process because eccentric exercises place less stress on the tendons than other types of strengthening exercises.
When eccentric exercises are applied to the joint, the exercises should be initiated within a shortened range of motion. Again, this is to ensure that the tendon is not placed in a position of stress during the earlier rehabilitation phases.
For example, when treating bicipital tendonitis, eccentric exercises should begin with the shoulder in a position of flexion. The arm is loaded in a position of flexion. The athlete resists moving the arm into extension, but the resistance is ended before the athlete’s shoulder is in full extension.
As the athlete’s strength improves, the athlete can move from endurance and eccentric types of strength exercises to concentric (shortening contraction) exercises focusing on gradually higher loads or intensities and fewer repetitions.
When can I begin functional sports training?
When strength exercises can be performed pain free and equal in intensity to the uninjured side, then the athlete can begin agility and functional sports specific training exercises. These exercises should be carefully selected to match the demands of the athlete’s sport.
For athletes recovering from lower extremity tendonitis, agility drills are introduced to ensure that the athlete’s body can respond quickly to demands for changes in direction. These drills should include a variety of directional changes and distances that mimic the demands of the athlete’s sport.
For example, an athlete competing in the sport of basketball recovering from patellar tendonitis should include agility drills that include the components of quickly shifting directions from side-to-side, front-to-back and back-to-front, and diagonal changes of directions all within small distances that would mimic the size of a basketball court.
Once agility drills can be performed pain-free and at a maximum intensity, functional sports specific drills can be performed. The keys to these drills is that they need to include all of the primary skills that the athlete needs to perform within their sport and that they gradually progress from low-intensity to high-intensity over time.
The basketball player recovering from patellar tendonitis should include non-contact sport specific drills like the following: defensive slides, line drills, shooting drills starting from shots close to the basket increasing to shots behind three point line, lay-ups, defensive drills, and offensive drills.
Once the athlete can complete all of these skills without pain, the athlete can then progress to contact drills. Once controlled contact drills can be performed without pain, the athlete can be released to full competition with no restrictions.
When can I return to sports?
The athlete can return to participation in sport when he/she has been released to participate by his/her sports medicine professional and is pain-free during full activity.
Chronic tendonitis is very difficult to treat. The goal for the athlete is to catch the tendonitis and treat it early before it becomes a chronic problem.
The keys to successfully treating tendonitis and returning an athlete to sport is early diagnosis, identification of the cause, addressing the cause, and following a careful progression of rehabilitation focusing initially on rest and reducing inflammation.
Diet and Nutrition Considerations for Treating Tendinitis
Understanding Calcific Tendonitis
What is Tendonitis? 🤔
.
.
.
#HazelGreenAL #Tendonitis pic.twitter.com/OXSxJ2zFlE— Hazel Green Chiropractic (@HazelGreenChir1) September 25, 2021
Reference
Houglum, P.A. (2005). Therapeutic Exercise for Musculoskeletal Injuries (2nd Ed.). Human Kinetics: Champaign, IL


