Elbow Bursitis
Last Updated on August 12, 2024 by The SportsMD Editors
Overview
Although an acute olecranon bursitis can look very traumatic, the injury itself is not serious and can be easily treated following the P.R.I.C.E. principles – Protection, Rest, Icing, Compression, Elevation – for acute injuries.
The body has a number of bursa in and around joints. Bursa are small fluid-filled sacs that act to decrease friction between soft tissues and bone. The bursa allows muscles and tendons to easily glide over boney prominences. However, when bursa become inflamed, motion at the affected joint may become painful and limited.
Bursitis is inflammation of a bursa. The injury can be either acute (one-time mechanism) or chronic (gradual inflammation caused by repetitive injury).
What is elbow bursitis?
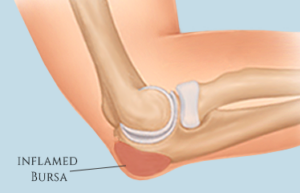 Although there are several small bursas located within the elbow, the olecranon bursa is the one that is the most prominent and commonly injured during sports. The olecranon bursa is located at the tip of the elbow off of the olecranon process of the humerus.
Although there are several small bursas located within the elbow, the olecranon bursa is the one that is the most prominent and commonly injured during sports. The olecranon bursa is located at the tip of the elbow off of the olecranon process of the humerus.
A subcutaneous olecranon bursitis in sports is most commonly an acute injury causing immediate swelling and deformity at the elbow. Because the olecranon bursa is the largest bursa in the elbow, when this bursa is injured, the function of the elbow can be significantly affected.
Signs and symptoms
An athlete with an acute injury would experience rapid signs and symptoms (within minutes) whereas an athlete with a chronic bursitis may develop signs and symptoms of the injury over several weeks.
The signs and symptoms include swelling directly over the tip of the elbow that may be mild, moderate or severe. The swelling may look something like a golf ball (mild swelling) or a tennis ball (moderate to severe) sitting on the tip of the elbow.
Although the inflamed bursa may not be painful itself, the increased pressure from the swelling may cause pain as the athlete tries to flex (bend) and straighten (extend) his/her elbow.
The danger in an olecranon bursitis is if the bursa becomes infected. If the bursa becomes infected, it is known as septic bursitis. This type of bursitis can actually be caused by an infection at another site (finger or hand) that travels up to the elbow.
The signs and symptoms of a septic bursitis are different from a nonseptic bursitis and will be similar to that of any infection in the body including the following:
• Fever
• Pain
• Localized heat
• Lethargy
• Restricted range of motion
• Tenderness
• Swelling
Diagnosis
Olecranon bursitis can be easily diagnosed by a thorough medical history and clinical evaluation by a sports medicine professional. Diagnostic tools are not necessary to diagnose this injury.
If a septic bursitis is suspected, the physician may aspirate the bursa and take a sample of the fluid for culture to determine if there is indeed infection in the bursa. After aspiration, the elbow is placed in a sling. Continuous heat packs are recommended along with antibiotics (Anderson, M.K., Parr, G.P., & Hall, 2009).
Who gets elbow bursitis?
The olecranon bursa is easily injured because it is located at the tip of the elbow and is not protected by muscle or soft tissue. Unfortunately, when an athlete falls, the elbow is exposed to injury due to its prominent location.
Any athlete competing in a sport who is at risk for falling on his/her elbow may be a candidate for possible olecranon bursitis. Another contributing risk factor to an acute bursitis is the type of surface that an athlete competes on. The harder and more dense the competitive surface (gym floor), the greater the athlete’s risk for sustaining an injury when the athlete falls.
With this in mind, athletes who are at risk for olecranon bursitis include those who compete in the sports of basketball and volleyball because they compete on hardwood floors and because these athletes hit the floor a lot.
Causes of elbow bursitis
An olecranon bursitis can be caused by a number of injury mechanisms including:
• A fall on a flexed elbow (acute)
• Repetitive pressure and friction (chronic)
• Repetitive flexion and extension (chronic)
Repetitive mechanisms would cause chronic bursitis injuries whereas a fall onto the tip of the elbow would cause an acute bursitis. According to Anderson, M.K., Parr, G.P., and Hall, S.J. (2009), there is an equal distribution of those that sustain injuries through one acute mechanism versus those that develop bursitis over time.
Prevention
To prevent a fall on the tip of the elbow, athletes need to be taught how to fall to safely protect their wrists, forearms, and elbows from injury. Athletes need to be taught to absorb the force of the fall by pulling their arms in and rolling. The athlete’s arms are tucked into the body with the goal of landing on the torso rather than on an extended arm.
The torso can more easily absorb the force of the body while the rolling dissipates the forces. This technique can prevent some of the most common injuries from falling on an outstretched arm including fractures, elbow dislocations, and wrist sprains.
To prevent chronic bursitis from constant loading on the olecranon bursa, elbow pads can be worn. Protective padding can prevent inflammation of the bursa through injury from constant pressure.
Elbow Bursitis Treatment
Elbow Bursitis is treated using the P.R.I.C.E. principles to reduce inflammation. Ice packs should be applied every two hours for twenty minutes for the first 48 hours. When the athlete is not applying ice, the elbow should be wrapped in an elastic bandage so that steady compression can be applied to the inflamed bursa.
If the bursa has severe inflammation, the physician may offer to aspirate the bursa. Once aspirated, the elbow is wrapped in a compression wrap for several days to ensure that the bursa does not become inflamed again.
Chronic bursitis is treated a bit differently with the focus on cryotherapy, NSAIDs, and the use of elbow padding to protect the elbow from further pressure. In some cases, a physician may recommend aspiration or the complete surgical removal of a chronically inflamed bursa.
Recovery – Getting back to Sport
The goal for recovery from an acute athletic injury bursitis is to decrease the inflammation so that the athlete can be pain free and have full range of motion of the elbow. The time frame for return to sport will be dependent on how long it takes for the bursitis to heal rather than by how many days the athlete is post-injury. Every athlete heals differently.
The ability for the athlete to safely return to sport will depend on the demands of the sport as well as the demands of the specific position. Athletes whose position and sport demands a full range of motion of the elbow (softball pitcher) may take longer to return to sport versus an athlete whose position and sport relies more on lower extremity ability and less upper extremity ability (football lineman).
Regardless of the sport, an athlete returning to sport after acute olecranon bursitis should wear some type of protective padding on the elbow either through a custom-made pad or through a commercial elbow pad.
When Can I Return to Play?
The athlete can safely return to sport when he/she has been released to return to play by his/her physician and has no swelling and pain-free full range of motion (complete flexion and extension equal to the uninjured elbow) of the elbow. The athlete should also be able to place their weight on the elbow without discomfort or pain.
Get a Virtual Sports Specialized appointment within 5 minutes for $29
 When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
When you have questions like: I have an injury and how should I manage it? How severe is it and should I get medical care from an urgent care center or hospital? Who can I talk to right now? SportsMD Virtual Urgent Care is available by phone or video anytime, anywhere 24/7/365, and appointments are within 5 minutes. Learn more via SportsMD’s Virtual Urgent Care Service.
Elbow bursitis is the inflammation of fluid-filled sac(s) that decrease friction between soft tissues and bines of the elbow. In athletes, it is caused by an acute injury causing immediate swelling and deformity at the elbow. #SportsMed #SportsCenter #physiotherapy pic.twitter.com/yzONVLshaZ
— Sports Medicine Professionals (@SportsmedicineP) November 6, 2020
Questions and Answers:
When discussing elbow bursitis or any medical condition with a doctor, asking questions can help you better understand your situation and treatment options. Here are some questions you can ask, along with potential answers from a healthcare professional:
- What is elbow bursitis?
- Elbow bursitis is a condition in which the bursa, a fluid-filled sac located around the elbow joint, becomes inflamed.
- What are the common causes of elbow bursitis?
- Elbow bursitis is often caused by repeated pressure or trauma to the elbow, such as leaning on it for extended periods or from acute injuries.
- How was elbow bursitis diagnosed in my case?
- Diagnosis typically involves a physical examination, medical history, and sometimes imaging studies, like X-rays or ultrasound.
- What symptoms should I expect with elbow bursitis?
- Common symptoms include pain, swelling, redness, and limited range of motion in the elbow area.
- What are the treatment options for elbow bursitis?
- Treatment options may include rest, icing, anti-inflammatory medications, physical therapy, draining the bursa, or, in rare cases, surgical removal of the bursa.
- How long will the recovery process take, and what can I expect during this time?
- Recovery time varies depending on the treatment approach and the individual. Your doctor can provide an estimate based on your specific case.
- Are there any potential complications associated with elbow bursitis or its treatment?
- Complications can vary, but are usually minor, such as infection at the site of bursal drainage. Your doctor can discuss these in detail.
- What is the long-term outlook for elbow bursitis?
- Most cases of elbow bursitis respond well to treatment, and patients can expect a full recovery.
- Do I need a follow-up appointment, and when should it be scheduled?
- Establish a plan for post-treatment follow-up appointments to monitor your progress and adjust the treatment plan if needed.
Always consult with your healthcare provider for personalized answers to these questions, and feel free to ask additional questions or seek clarification on any points you don’t fully understand. Effective communication with your doctor is essential for your understanding and overall care.
References
- Anderson, M.K., Parr, G.P., & Hall, S. (2009). Foundations of Athletic Training: Prevention, Assessment, and Management. (4th Ed.). Lippincott Williams & Wilkins: Baltimore, MD.
- Rouzier, P. (1999). The Sports Medicine Patient Advisor. SportsMed Press: Amherst, MA.

