Herniated Disk or Bulging Disk
Last Updated on October 23, 2023 by The SportsMD Editors
Herniated or bulging disks are relatively common in the field of sports medicine and can affect athletes involved in many different sports. Although the mechanisms of the injury are slightly different depending on which section of the spine they occur, the outcomes are the same.
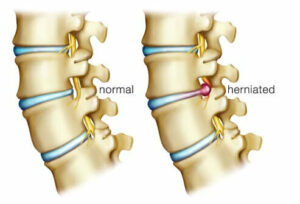
To understand what a herniated disk is, there needs to be a basic understanding of what an intervertebral disk is and how it functions within the spinal column. Intervertebral disks lie between all of the cervical, thoracic, and lumbar vertebrae. Each disk is made up of two components. The structure of each part of the disk dictates its function.
The inside portion of the disk is called the nucleus pulposus and is composed of a highly viscous semifluid material. One can think of this material as a thick gel pad sandwiched in between the vertebrae for the purpose of providing shock absorption for the forces transmitted down the spine.
 The outer portion of the disk is made up of strong, fibrous tissue called the annulus fibrosis. These thick fibers circle the nucleus pulposus and provide the outer boundaries of the intervertebral disk. Although helping with the shock absorption along with the nucleus pulposus, the annulus fibrosis also plays a role in restricting rotational movement between each vertebrae.
The outer portion of the disk is made up of strong, fibrous tissue called the annulus fibrosis. These thick fibers circle the nucleus pulposus and provide the outer boundaries of the intervertebral disk. Although helping with the shock absorption along with the nucleus pulposus, the annulus fibrosis also plays a role in restricting rotational movement between each vertebrae.
A herniated disk occurs when there is a tear in the outer portion of the disk (annulus fibrosis) with the nucleus pulposus material oozing out from the disk. Although there are varying classifications and degrees of disk injuries, the worst-case scenario is that the material from the inside of the disk leaks out and puts pressure on one of the spinal nerves. This can result in varying degrees of neurological symptoms including weakness, burning, numbness, and tingling of the associated nerve pathway/extremity.
Classifications of herniated disks
There are four distinct classifications of herniated disks moving from mild to severe depending on how far the nucleus pulposus has moved from its original position in the center of the disk.
First classification is bulging disk or a protruding disc:
This occurs when the inner gel-like material of the nucleus pulposus extends beyond its origin and moves into the fibers of the annulus fibrosis.
Second classification is prolapsed disk:
If the nucleus pulposus continues to move through the fibers of the annulus fibrosis it is then considered a prolapsed disk. In this case, the nucleus material is still contained with the annulus fibrosis, but it has worked its way all the way through to the outer border of the disk.
Third classification is extruded disk:
When the nucleus material moves beyond the borders of the annulus fibrosis and into the spinal canal, it is called an extruded disk. It is at this point when the individual may start feeling some neurological effects from the disc herniation as the nucleus pulposus compresses one or more nerve roots or other soft tissue structures.
Fourth classification is sequestrated disk:
The most severe type of herniated disc is called a sequestrated disk. This is defined as when the nuclear material has separated from the disc itself with the risk being that the gel-like material may migrate.
The intervertebral disk itself does not have any sensory innervation. In other words, the disk itself cannot feel pain. This is a good thing under normal circumstances because the disk is subject to constant compressive loading of the adjacent vertebrae anytime an athlete is in an upright position.
When the nucleus pulposus begins to extend beyond its natural boundaries, there is initially no pain involved. The pain and symptoms of a herniated disk only begin when the material of the disk begins to extend beyond the annulus fibrosis and pushes against soft tissues that have sensory nerve innervation.
It is not unusual to have individuals walking around with either protruded or prolapsed discs with no pain or neurological symptoms.
Symptoms of herniated disk
The general types of signs and symptoms of a herniated disk will be similar regardless of the level of the disk injury. However, the level of the disk injury will dictate which extremities are affected.
Symptoms may include sharp pain and muscle spasms in the vicinity of the herniated disk. Neurological symptoms may also include shooting pain, radiating pain, weakness, burning, tingling, and numbness following the nerve root that is affected by the herniation.
In the area of the neck, these symptoms may follow nerve roots and cause pain into the shoulder, arm, and fingers. The individual may experience numbness/tingling in the fingers with associated muscle weakness of the involved nerve root. Associated reflexes may also be involved.
In the lumbar area, the individual may experience radiating pain down the back of the hip and all the way down the leg. The individual may walk slightly crouched over with a lean towards the opposite side of the herniation. This position helps take the pressure off the herniated disk.
The most common herniated disks in the lumbar region are between L4-L5 and L5-S1. A herniation to the intervertebral disc between L4 and L5 would have the following symptoms:
• Low back pain, groin pain, and pain to the sacroiliac area (back of pelvis)
• Sensory loss of lateral thigh, front of leg, top of the foot, and middle three toes
• Muscle weakness in great toe extension (pulling big toe up)
• Reduced medial hamstring tendon reflex
A herniation to the intervertebral disc between L5 and S1 would have the following symptoms:
• Pain in the low back, groin, and sacroiliac area (back of pelvis)
• Sensory loss in posterior lateral thigh and lower leg to lateral foot and fifth toe
• Muscle weakness in plantar flexion (going up on toes)
• Reduced achilles tendon reflex
Diagnosis of herniated disk
A thorough and careful clinical assessment can determine if there is a disk herniation specifically looking for nerve root involvement including radiating pain, weakness, sensory deficits, and abnormal reflex tests. To confirm the diagnosis, the sports medicine physician may order an MRI, x-rays, or an electromyogram nerve stimulation study (measures activity within specific muscles to determine if there is sufficient motor nerve stimulation of the muscle).
Who gets a herniated disk?
Cervical disk injuries usually affect older, physically active individuals. In this case, these individuals may be affected by a chronic, degenerative disk disease. Over time, the disk height diminishes and there may be the formation of bony growths known as osteophytes in and around the vertebrae.
Acute cervical disk injuries can be seen in athletes who compete in contact sports and who receive repetitive axial loading (compression forces through the head and the spine) or hyperflexion type injuries such as seen in the sport of football. Athletes who lead with their heads may be at risk for a cervical disc injury.
In the lumbar spine, disc injuries can occur in athletes who repetitively load their spine and combine the movement with a twist or lateral bending move. This can be seen in the sport of basketball when an athlete comes down from a rebound and then twists the upper body to clear the area of any nearby defenders.
Causes of herniated disk
The best way to explain the causes of a herniated disk is to think of the disk as a gel-filled balloon. The disk is sandwiched above and below by the bodies of two adjacent vertebrae. When compressive loads are distributed equally across the vertebrae, then the disk has an equal amount of force spread throughout the disk. This is a good and healthy position for the disk.
However, when an individual twists and then performs a lateral bend, the vertebrae on one side of the body are compressed while the vertebrae on the opposite side are extended. The portion of the disk on the compressed side of the vertebrae is compressed just like that of a balloon when one side is compressed.
If the force is great enough on the side of the vertebrae and disk being compressed, then the outside of the disk can tear allowing the nucleus gel-like substance to leak out. The spine is at its weakest and the disk is at its greatest risk of injury during flexion, rotation, and lateral bending movements of the spine.
Prevention for herniated disk
Prevention of a herniated disk begins with education on proper mechanics when lifting or using the back. The disk is safest and most protected when the spine is in neutral (straight up and down). This is the position that should be maintained when lifting heavy objects.
Individuals need to be taught to lift with the large muscles of the buttocks and thighs while keeping the spine straight and the core muscles co-contracted. This position keeps the disk out of harm’s way while the spine is being externally loaded.
For athletes and active populations, developing and maintaining core strength is the key to protecting the intervertebral disks. Tight core muscles surrounding the vertebrae can assist in protecting the disks by providing an extra layer of protection immediately around the motion segments of the spine. Strong muscles can prevent unwanted or excessive movement of the spine.
Along with strengthening the muscles surrounding the vertebrae, educating athletes as to the mechanisms that may cause disk herniation is also important. Teaching athletes proper mechanics within their sport is integral in preventing serious injuries to the spine and associated structures.
Treatment for herniated disk
Initial treatment for most herniated disks is a conservative approach initially focused on reducing any associated muscle spasms. This can be accomplished through the following:
• Rest
• Immobilization in a cervical collar (for cervical intervertebral disk herniation) for one to three days
• Activity modification (avoiding bending, lifting, twisting, and prolonged sitting or standing)
• Administration of NSAIDs and/or muscle relaxants
As the muscle spasm releases, gentle stretching of the spine and hamstring muscle groups can be started. Isometric muscle contractions (contractions with no movement) for the spine can also be started early in the rehabilitation.
One isometric exercise that is good early in the rehabilitation process is the supine Pelvic Tilt. This is performed with the individual lying down on the floor with their hips and knees bent (feet on the floor). The individual then presses their lower back to the floor and holds this position for 10 seconds. Initially, the individual may only be able to hold this contraction for three to five seconds.
The goal is to work up to 10 repetitions of 10 seconds every hour. This type of exercise engages the erector spinae muscles without ever having to move the spine. The individual can begin the contractions at 50% of intensity and then gradually work up to full intensity as their strength improves.
Once the individual can move their spine without pain, additional spine strengthening and stabilization exercises can be added. The goal for these exercises is to strengthen the muscles surrounding the spine including the abdominal muscles (responsible for flexing the spine), the internal and external oblique muscles (responsible for twisting and lateral bending), and the erector spinae (responsible for extending the spine).
Once the athlete has obtained pain-free full range of motion and full strength in all of the core muscles, the athlete can then begin sport-specific functional training.
Although the initial treatment goal is conservative, if the symptoms do not resolve, then the athlete may need surgical intervention to alleviate the pressure of the herniation on the nerve roots and/or soft tissue structures.
Recovery – Getting back to Sport
Sports-specific activities and drills can be started when the athlete has regained full strength and pain-free mobility. Before an athlete can be released to return to his/her sport, the athlete needs to have confidence in his/her ability to perform at intense levels without the fear of pain.
In order to accomplish this goal, the athlete begins a progressive series of functional training exercises that mimic what the athlete will perform during his/her sport. The progressions should start at about 50% of intensity and initially without any sport implements/gear.
All sports skills that the athlete may be engaged in should be included in these activity progressions. As the athlete’s confidence increases, the intensity of the activities can gradually increase until the athlete is performing at full intensity.
When Can I Return to Play?
The athlete can return to play when the athlete has been released to return to sports by a sports medicine professional and when he/she has the following:
• Full pain-free range of motion
• Full strength
• Full power
• No neurological symptoms
• Completion of sport-specific functional training
Get a Telehealth Appointment or Second Opinion With a World-Renowned Orthopedic Doctor
 Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
References
- Anderson, M.K., Hall, S.J., & Martin, M. (2005). Foundations of Athletic Training: Prevention, Assessment, and Management. (3rd Ed.). Lippincott Williams & Wilkins: Philadelphia, PA.
- Arnheim, D.D. & Prentice, W.E. (2000). Principles of Athletic Training. (10th Ed.). McGraw Hill: Boston, MA.
- Bahr, R. & Maehlum, S. (2004). Clinical Guide to Sports Injuries. Human Kinetics: Champaign, IL.
- Irvin, R., Iversen, D., & Roy, S. (1998). Sports Medicine: Prevention, Assessment, Management, and Rehabilitation of Athletic Injuries. (2nd Ed.). Allyn and Bacon: Needham Heights, MA.
- Kibler, W.B., Herring, S.A., Press, J.M.,& Lee, P.A. (1998). Functional Rehabilitation of Sports and Musculoskeletal Injuries. Aspen Publication: Gaithersburg, MA.
- Starkey, C. & Ryan, J. (2002). Evaluation of Orthopedic and Athletic Injuries. (2nd Ed.). F.A. Davis: Philadelphia, PA.

