Shoulder Instability
Last Updated on October 21, 2023 by The SportsMD Editors
The term “shoulder instability” constitutes a spectrum of disorders that includes dislocation, subluxation and laxity. When the shoulder slips partially out of joint, this is called subluxation. A dislocated shoulder occurs when the shoulder comes completely out of joint. There are some people who have a capsule that is a little bit too loose.
Such individuals are described as having ligamentous laxity or being “lax”. It should be noted that laxity is a variation of normal whereas instability is not. Therefore, patients can have baseline laxity and then suffer an injury that leads to instability.
Causes shoulder instability
The capsule that surrounds the shoulder joint is a very strong ligament that helps to keep the shoulder in the joint and functioning normally. In most people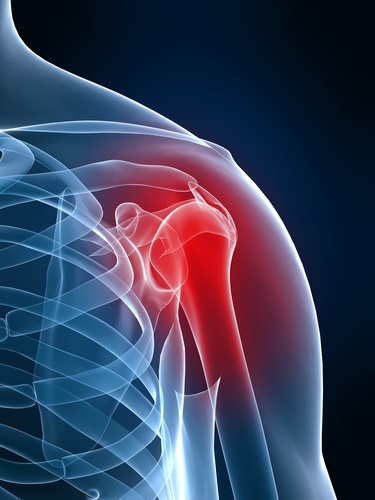 it is very difficult to tear the ligaments of the capsule and cause the shoulder to dislocate. These injuries usually occur only when a lot of force has been applied to the shoulder or the arm — like in a tackle football game. If the shoulder slips in and out of joint more than once or twice, or frequently slips partially out of joint and then returns on its own, then the joint is said to be “unstable”. This condition can create a lot of problems for patients because they may not be able to do certain activities because they are afraid their shoulder will slip out of joint if they move their arm into certain positions. This is a particularly big problem for people who work with their hands above their heads like baseball pitchers and tennis players who depend upon their shoulder to play certain sports. Contact athletes (football, rugby, etc…) are also at high risk. Lastly, there is also a concern that the surface cartilage of the shoulder can be damaged if it slips in and out of joint frequently.
it is very difficult to tear the ligaments of the capsule and cause the shoulder to dislocate. These injuries usually occur only when a lot of force has been applied to the shoulder or the arm — like in a tackle football game. If the shoulder slips in and out of joint more than once or twice, or frequently slips partially out of joint and then returns on its own, then the joint is said to be “unstable”. This condition can create a lot of problems for patients because they may not be able to do certain activities because they are afraid their shoulder will slip out of joint if they move their arm into certain positions. This is a particularly big problem for people who work with their hands above their heads like baseball pitchers and tennis players who depend upon their shoulder to play certain sports. Contact athletes (football, rugby, etc…) are also at high risk. Lastly, there is also a concern that the surface cartilage of the shoulder can be damaged if it slips in and out of joint frequently.
Are there different types of shoulder instability?
Most clinicians classify instability by direction. Anterior (towards the front of the body) is by far the most common. Patients can also suffer from posterior (towards the back of the body) instability or multidirectional instability where the shoulder is unstable in the anterior, posterior, and inferior directions. Distinguishing between the different types of instability is important because different types will often have different treatment options.
Who gets shoulder instability?
Generally speaking, shoulder instability tends to occur in three types of patients
(1) Patients who have sustained a prior shoulder dislocation often develop chronic shoulder instability. In these patients, the ligaments that support the shoulder are torn when the dislocation occurs. If these ligaments heal too loosely, then the shoulder will be prone to repeat dislocation and episodes of instability. When younger patients (less than about 35 years old) sustain a traumatic dislocation, chronic shoulder instability will follow in about 80% of patients despite physical therapy.
(2) Athletes who compete in sports that involve overhead activities can develop multidirectional instability (MDI) as a result of their sporting activities. These athletes, such as volleyball players, swimmers, and baseball pitchers, stretch out the shoulder capsule and ligaments, and may develop chronic shoulder instability. While they may not completely dislocate the joint, the apprehension, or feeling of being about to dislocate, may prevent their ability to play these sports
(3) Patients with some connective tissue disorders may have loose shoulder joints. In patients who have a condition that causes joint laxity, or double-jointedness, their joints may be too loose throughout their body. These patients can suffer from multiple joint dislocations including most commonly the patella and the shoulder.
How do I know if my shoulder is unstable?
In cases of frank shoulder dislocations, the diagnosis is usually obvious. More subtle degrees of instability will require a thorough history and physical examination. The goal of the physical examination is to determine in which direction the shoulder slips out of joint, and how loose the injured shoulder is in comparison to the other one. X-rays and MRI are obtained to assess for areas where the ligaments of the capsule have been torn or damaged. (need picture of an Xray demonstrating Hill Sachs lesion and a picture of MRI demonstrating Bankart lesion)
Treatment of shoulder instability
The most important thing initially is to demonstrate that the shoulder is concentrically reduced (x-rays). Once a concentric reduction has been confirmed, treatment of shoulder instability depends on several factors, and almost always begins with physical therapy and rehab. If patients complain of a feeling that their shoulder is loose or about to dislocate, physical therapy with specific strengthening exercises will often help maintain the shoulder in proper position. Other treatments sometimes used to treat shoulder instability can include occasional anti-inflammatory medications. Cortisone injections should be discouraged.
What is the role of physical therapy?
Physical therapy can play a significant role in preventing recurrent instability by strengthening the surrounding shoulder musculature to help keep the shoulder reduced. The athletic population that probably most benefits from physical therapy are those that have multidirectional instability where the instability is from generalized capsular laxity as opposed to unidirectional instability (anterior or posterior) where the instability is caused by tearing of the ligaments or capsule away from the bone.
When do I need surgery?
Any patient who continues to have recurrent dislocation or feelings of instability during sporting activities despite extensive physical therapy and rehabilitation are candidates for surgery.
What is the goal of surgery?
Post-traumatic shoulder instability can be corrected with surgical procedures that are designed to repair and strengthen the ligaments that keep the shoulder in the joint normally. These operations have been developed over the years as doctors have recognized that many unstable shoulders have a particular type of injury called a “Bankhart lesion”. The Bankhart lesion specifically refers to an injury where part of the capsule of the shoulder joint is pulled away from the bone. Surgical techniques are aimed at fixing this problem and also tightening up the ligaments of the shoulder that have been stretched or torn by the dislocation. Repairing the torn capsule and ligament back to the bone is called a Bankhart repair, and tightening the capsule of the shoulder is called a “capsular shift”. It should be noted that patients who suffer from multidirectional instability rarely have a Bankhart lesion. Therefore, the surgical procedure consists of a capsular shift only.
Should I have “open surgery” or arthroscopic surgery?
All of the surgical procedures used to treat all types of shoulder instability can be done either open or arthroscopically. The advantage of open techniques is that they have a longer track record so to speak and many surgeons have more experience using this technique. Also, most published studies show a lower rate of recurrence using open techniques. The advantage of arthroscopic techniques is that they are much less invasive, patients have less pain after the surgery, and can recover quicker. (need a video of arthroscopic anterior stabilization) The disadvantage is that some clinicians have less experience using arthroscopic techniques and they do appear to have a higher recurrence rate compared to open techniques. It is difficult to generalize which technique is best suited for each individual patient. Your doctor will be able to discuss the advantages and disadvantages of the different types of surgery that are designed to correct shoulder instability.
When can I expect to return to sports after surgery?
Regardless of which type of surgery the patient has, most clinicians will discourage competitive sports for at least 4 months. Patients who wish to participate in contact sports (football, soccer, rugby) are generally not permitted to play for at least 6 months.
How likely is it that my shoulder will dislocated or subluxate again after surgery?
Most studies suggest that the likelihood of recurrent instability is anywhere from 5-10 percent after open surgery and 2-25 percent after arthroscopic surgery.
Get a Telehealth Appointment or Second Opinion With a World-Renowned Orthopedic Doctor
 Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
- Bahr R, Craig EV, Engebretsen L. The clinical presentation of shoulder instability including on field management. Clin Sports Med 1995;14:761-76.
- Allen AA, Warner JJ. Shoulder instability in the athlete. Orthop Clin North Am 1995;26:487-504.
- Tibone JE, Bradley JP. The treatment of posterior subluxation in athletes. Clin Orthop 1993;291124-37.
- Yamaguchi K, Flatow EL. Management of multidirectional instability. Clin Sports Med 1995;14:885-902.
- Arciero RA, St. Pierre P. Acute shoulder dislocation. Indications and techniques for operative management. Clin Sports Med 1995;14:937-53.
- Guanche CA, Quick DC, Sodergren KM, Buss DD. Arthroscopic versus open reconstruction of the shoulder in patients with isolated Bankart lesions. Am J Sports Med 1996;24:144-8.

