IT Band Syndrome
Last Updated on October 22, 2023 by The SportsMD Editors
IT Band Syndrome is an overuse injury that is common in athletes including runners, cyclists, volleyball and basketball players. 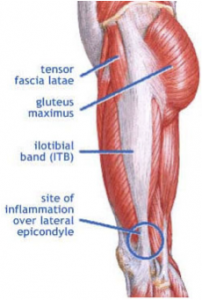 The iliotibial band (IT band) is a long flat fibrous band that runs all the way down the outside of the thigh connecting the tensor fasciae latae muscle (originates in the pelvis) to the anterior tibia just below the knee.
The iliotibial band (IT band) is a long flat fibrous band that runs all the way down the outside of the thigh connecting the tensor fasciae latae muscle (originates in the pelvis) to the anterior tibia just below the knee.
Most muscle/tendon units are made up primarily of muscle with smaller tendon attachments. However, the tensor fasciae latae/IT band is an unusual musculotendinous pair because the muscle is very small as compared to the long length of the IT band.
It is specifically this anomaly that creates the friction problem down in the knee area. If the IT band is tight, the IT band can rub and snap across the lateral femoral epicondyle when the knee moves from a flexed position into an extended position. This is exacerbated when the athlete is weightbearing as in the activities of running, cycling, and jumping.
Who gets IT band syndrome?
Athletes who use a lot of flexion and extension in their sport are most at risk for iliotibial band syndrome. These would include athletes in the sports of long-distance running, cycling, volleyball, basketball, and weight lifting.
Classifications of IT band syndrome
Iliotibial band syndrome can be classified as either mild, moderate, or severe depending on the intensity and duration of the symptoms. The pain is usually localized over the lateral condyle of the femur just above the lateral joint line of the knee. The pain may also radiate either up the IT band to the hip or down the IT band to its insertion on the tibia.
Athletes who experience pain towards the end of their activity and in which they are still able to continue would be classified as having a mild iliotibial band syndrome. The pain may be more noticeable during the phase of heal strike through mid-stance when the IT band is in its tightest position between the greater trochanter of the femur and the lateral femoral epicondyle.
As the condition worsens, the athlete may feel pain earlier and earlier during his/her activity. The pain will eventually affect the athlete’s ability to continue. The athlete may also begin to feel pain during weight-bearing activities such as walking down a flight of stairs. This would be classified as a moderate iliotibial band syndrome.
The condition is classified as severe when the pain restricts all running and becomes constant throughout all activities during the day.
Diagnosis
A sports medicine professional can diagnose iliotibial band syndrome given a thorough medical history and comprehensive physical assessment. There are two special tests that can be used to help diagnose this syndrome.
First test Noble Compression
The athlete lies on a table with his/her hip and knee flexed. The athlete slowly extends the injured leg while pressure is applied to the IT band just proximal to the lateral epicondyle of the femur. If the test is positive, the athlete would have significant pain while straightening his/her leg.
Second test Ober’s
The athlete lies on his/her uninjured side with the leg in slight flexion to help maintain balance. The injured leg is passively abducted and slightly extended and then slowly brought back down. If the IT band is tight, the leg will remain in an abducted position.
Causes of IT band syndrome
As an athlete uses his/her legs in repetitive motions, the IT band can become tight. Athletes often focus on stretching the muscles of the hip and thigh, but stretching the IT band is not often included in an athlete’s general warm-up protocol. This structure can become tight without the athlete realizing the problem until the pain hits.
A number of factors can predispose an athlete to iliotibial band syndrome including the following:
• Excessive pronation of the feet
• Leg-length discrepancy
• Prominent greater trochanter of the femur
• Training errors such as excessive distance in a single run, increasing mileage too quickly, inadequate warm-up, and running on the same side of a crowned road
Excessive pronation of the feet
This means that the athlete’s foot or feet roll inward towards each other when he/she walks or runs which translates upwards into the knee. This places additional strain on the IT band to control this excessive internal rotation and accompanying adduction with each footstep. This can easily be determined by watching the individual walk a short distance from behind the athlete. If the medial ankle bones roll downwards and towards each other, then the athlete is a pronator. This problem of over-pronation can be easily corrected. If it is only a minor problem it can normally be corrected by visiting a specialist sports shop where they should be able to advise you on a pair of running shoes with built in support to alter your foot position. If the pronation is more marked you may need to invest in a good pair of orthotics which are placed into the shoes and trainers to correct the foot position.
Leg-length discrepancy
A sports medical professional can measure an athlete for leg-length discrepancy. If the athlete does have one leg shorter than the other, the athlete can be referred for corrective shoes. Unfortunately, there is nothing that can be done for a prominent greater trochanter.
Training errors
Can also be easily corrected and the athlete needs to ensure that he/she includes a sufficient and gradual warm-up prior to intense activities. If the athlete is a runner, the athlete should pay specific attention to the level of the surfaces upon which he/she runs. Those who run on the edge of the road where one foot is then lower are also vulnerable to the condition. This is because the foot hitting the lower part of the road has to travel a further distance each time it hits the ground. This is the same effect as having a leg length difference.
Prevention
One of the most effective ways to prevent iliotibial band syndrome is to keep the IT band stretched and loose. Although this can be done manually by a sports medicine professional, it can also be accomplished through the use of a foam roller.
The foam roll should be placed on a carpeted surface perpendicular to the athlete. The bodyweight of the athlete provides the force to stretch the IT band. The athlete lies down on the side of the injured leg placing the foam roll at the level of the knee. The athlete then slowly pushes his/her body weight across the foam roll until the roll is at the level of his/her hip. Then the athlete reverses directions and slowly rolls back across the foam roll until the foam roll is back at the knee.
The athlete should know that this can be an uncomfortable exercise because of the pain experienced when the tight IT band rolls on the foam roll. If it is too uncomfortable, then the athlete can take some of his/her bodyweight off of the roll by moving the top leg back or by lifting the upper body up a bit with the arms thereby reducing the amount of weight on the foam roll.
Treatment
The athlete needs to understand that continuing to compete and exercise with iliotibial band syndrome will make the condition worse. Because iliotibial band syndrome is a repetitive overuse-type of injury, the first thing the athlete needs to do is rest the knee. Rest will allow the inflammatory process to run its course eliminating the inflammation and swelling in the area.
If complete rest is not an option, then the athlete’s activities should be modified to reduce the amount of weightbearing flexion/extension of the knee. For runners, this might include resting from running, but getting a cardiovascular workout by swimming or using a bike. For volleyball or basketball players, this might include reducing the number of jumping/landing drills during practice.
Ice massage or is an effective modality to reduce swelling and pain for this injury. Although commercial ice cups are available, an ice cup can easily be made at home by freezing water in a Styrofoam cup. When the water has frozen, remove the ice cup from the freezer, peel off the top inch of the Styrofoam cup, and then rub away the sharp top edges by melting the edges against the athlete’s hand.
After placing a towel under the knee, the athlete can massage the tender area by gently applying pressure beginning at the knee and slowly moving the ice cup towards the hip through the painful area. This can be done for 10 minutes both before and after exercise/practice.
Stretching the IT band daily will gradually loosen the tight tissue.
When can I return to sports?
Ideally, the athlete should have pain-free weight-bearing range of motion of the knee before returning to sports. Continuing to play or compete through pain will only elongate the healing process.
Get a Telehealth Appointment or Second Opinion With a World-Renowned Orthopedic Doctor
 Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
Telehealth appointments or Second Opinions with a top orthopedic doctor is a way to learn about what’s causing your pain and getting a treatment plan. SportsMD’s Telehealth and Second Opinion Service gives you the same level of orthopedic care provided to top professional athletes! All from the comfort of your home.. Learn more via SportsMD’s Telemedicine and Second Opinion Service.
Recent articles on IT Band Syndrome
IT band syndrome and plantar fasciitis are two other pesky syndromes that could go hand-in-hand (foot-in-foot?) with over-worn sneaks. That’s why, when looking for a new pair, you should always seek a professional opinion on the right style for you. 5 Signs Your Body Is Trying To Tell You It’s Time To Ditch Your Old Sneakers – Elite Daily

